Lancet:全球半数病例在中国,K药为食管癌患者带来好消息!
2021-08-29 MedSci原创 MedSci原创
食管癌是一种常见且预后较差的癌症。在全球范围内,食管癌是导致癌症死亡的第五大原因。
食管癌是一种常见且预后较差的癌症。在全球范围内,食管癌是导致癌症死亡的第五大原因。而中国的食管癌发病和死亡病例占到全球近一半,食管癌也是中国第四大癌症死亡原因。
为了更好地为食管癌的预防、治疗和护理提供信息,《柳叶刀-胃肠病学和肝病学》发表了全球195个国家地区的食管癌发病率、死亡率和可归因风险因素等最新统计数据。由于统计数据通常存在一定滞后性,研究数据源于2017全球疾病负担研究。
报告显示,中国的食管癌发病和死亡负担占到全球近一半,并提示了与日常生活息息相关的五大危险因素。食管鳞状细胞癌和食管腺癌是两种主要组织学亚型。报告显示,社会人口指数(SDI)、医疗可及和质量(HAQ)指数较低,同时室内空气污染水平较高的国家,食管鳞状细胞癌占所有食管癌病例的比例较高。
根据中国国家卫健委公布的《食管癌诊疗规范(2018年版)》,中国食管癌以鳞状细胞癌为主,占90%以上。而2017年食管癌可归因于5个已知的危险因素,包括:吸烟(39.0%)、饮酒(33.8%)、高体重指数(BMI)(19.5%)、饮食中水果摄入量低(19.1%)和咀嚼烟草(7.5%)。
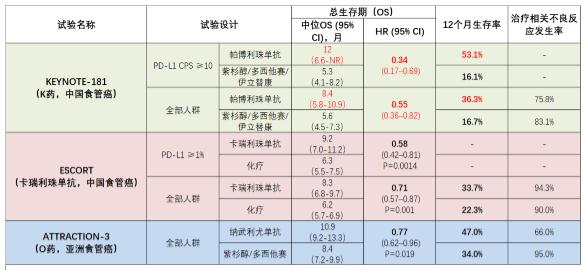
目前,晚期食道癌的一线治疗仅限于氟嘧啶加铂类化疗,因此晚期食管癌的死亡率很高。近期,来自韩国成均馆大学三星医疗中心的专家旨在评估PD-1抗体帕博丽珠单抗(K药)加化疗与单纯化疗作为晚期食道癌和胃食管交界处癌的一线治疗的抗肿瘤活性。结果发表在Lancet杂志上。
研究人员在26个国家的168个医疗中心做了一项随机、安慰剂对照、双盲、3期研究。年龄在18岁或以上,先前未经治疗,经组织学或细胞学证实的局部晚期、不可切除或转移性食道癌或胃食道交界处癌的患者。随机分配(1:1)到静脉注射K药200mg或安慰剂,加上5-氟尿嘧啶和顺铂(化疗),每3周一次,最多35个周期。随机化是按地理区域、组织学和表现状态分层的。主要终点是食道鳞状细胞癌和PD-L1联合阳性评分(CPS)为10或以上的患者的总生存期,以及食道鳞状细胞癌、PD-L1 CPS为10或以上的患者和所有随机患者的总生存期(OS)和无进展生存期(PFS)。
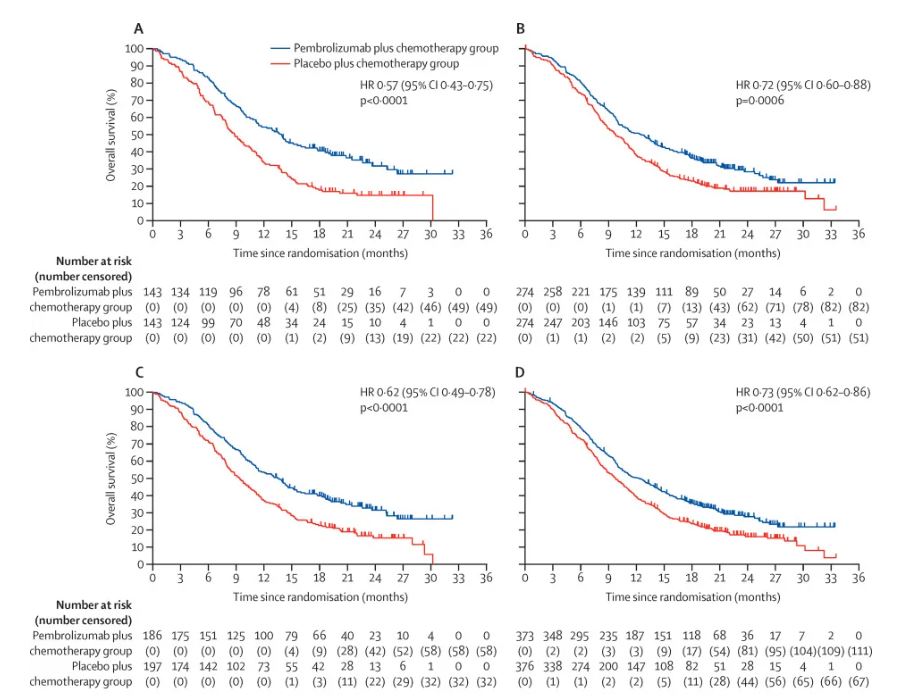
在2017年7月25日至2019年6月3日期间,1020名患者被筛选,749名患者入选,并随机分配到K药加化疗(n=373[50%])或安慰剂加化疗(n=376[50%])。在第一次中期分析中(中位随访22.6个月),K药加化疗在食道鳞状细胞癌和PD-L1 CPS≥10的患者的总生存率方面优于安慰剂加化疗,死亡风险降低43%(中位13.9 vs 8.8个月;OR=0.57,95% CI:0.45-0.73);同样,食道鳞状细胞癌患者死亡风险降低28%(12.6 vs 9.8个月;OR=0.72);PD-L1 CPS≥10降低38%(13.5 vs 9.4个月;OR=0.62)。
不同亚组接受帕博利珠单抗联合化后的OS。(A)食管鳞癌且PD-L1 CPS≥10,(B)食管鳞癌,(C)PD-L1 CPS≥10,(D)所有随机分组的患者
此外,所有随机患者延长了OS,死亡风险降低27%(12.4 vs 9.8个月;OR=0.73)、延缓复发,延长无进展生存期(6.3个月 vs 5.8个月),进展或死亡风险降低35%;24个月总生存率更高(28% vs 16%)。
综上,与安慰剂加化疗相比,K药加化疗改善了先前未治疗的晚期食道鳞状细胞癌和PD-L1 CPS≥10的患者的总生存期,以及食道鳞状细胞癌、PD-L1 CPS≥10的患者的总生存期和无进展生存期,并且在所有随机患者中,无论何种组织学,都具有可控的安全状况。
参考文献:
Pembrolizumab plus chemotherapy versus chemotherapy alone for first-line treatment of advanced oesophageal cancer (KEYNOTE-590): a randomised, placebo-controlled, phase 3 study. https://doi.org/10.1016/S0140-6736(21)01234-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Lancet#
26
#食管癌患者#
48
#食管#
19
#K药#
39
收藏了,谢谢
47
顶刊就是不一样,质量很高,内容精彩!学到很多
29