Aliment Pharmacol Ther:美研究发现丙肝疾病进展预测因子
2014-11-13 伊文 生物谷
丙型肝炎(hepatitis C)临床治疗的巨大进步,已使得越来越多的患者积极寻求治疗,随之也出现了关于如何向所有患者提供治疗的后勤和财政方面的担忧。 美国密歇根大学健康系统的一支研究团队,对相关文献进行了系统回顾,旨在确定关于丙肝疾病进展(纤维化进展和临床结果)的预测因子,并评估现有的预测模型。 方法:对MEDLINE、PUBMED、EMBASE、Web of
丙型肝炎(hepatitis C)临床治疗的巨大进步,已使得越来越多的患者积极寻求治疗,随之也出现了关于如何向所有患者提供治疗的后勤和财政方面的担忧。
美国密歇根大学健康系统的一支研究团队,对相关文献进行了系统回顾,旨在确定关于丙肝疾病进展(纤维化进展和临床结果)的预测因子,并评估现有的预测模型。
方法:对MEDLINE、PUBMED、EMBASE、Web of Science、Scopus数据库中从2003年1月-2014年6月发表的研究报告进行全面搜查。对这些文章进行审查,选择符合条件的研究,进行数据抽取。
结果:29个研究代表了来自20个队列的5817例患者纳入了分析。每种结果发生率(outcome incidence rates,OIR)变化都很大:纤维化进展在中位随访2.5-10年期间发生率16-61%;肝功能失代偿中位随访2.3-14.4年发生率13-40%;总死亡率在3.9-14.4年发生率8-47%。
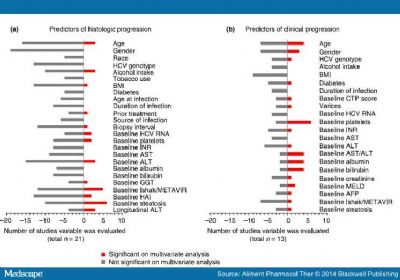
多变量分析显示,基线脂肪变性和基线纤维化评分是肝纤维化进展最一致的预测因子(分别在6/21、5/21研究中显著);基线血小板计数(在6/13研究中显著)、天冬氨酸/谷丙转氨酶(AST/ALT)比值、白蛋白、胆红素、年龄(每一项分别在4/13研究中显著)是临床结果最一致的预测因子。5项研究建立了预测模型,但均未被外部验证。
结论:发现了关于丙肝疾病进展最一致的预测因子,并建立了基于风险的方法,能够帮助辨认需要及时治疗和密切监测的丙肝患者,有望使资源和药物有效利用达到最大化。
原始出处:
M. A. Konerman, S. Yapali, A. S. Lok.Identifying Patients With Chronic Hepatitis C in Need of Early Treatment and Intensive Monitoring:Predictors and Predictive Models of Disease Progression.Aliment Pharmacol Ther. 2014;40(8):863-879.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#MAC#
0
#pharma#
41
#Pharmacol#
35
#Pharm#
31
#研究发现#
39
#疾病进展#
28
#预测因子#
0