Front Oncol:分析术前放疗对比术后放疗对局部晚期乳腺癌(LABC)患者的总生存影响
2021-11-29 yd2015 MedSci原创
研究表明,局部晚期乳腺癌(LABC)患者术后放疗可改善患者预后。术前放疗并不能比术后放疗改善患者预后。
局部晚期乳腺癌(LABC)的治疗是一个棘手的临床问题。术后放疗是LABC患者的常规治疗方法,而术前放疗对LABC预后的影响仍存在争议。因此,国内团队开展了回顾性研究,旨在分析和比较LABC患者术前放疗和术后放疗的总生存期(OS)差异。相关结果发表在Frontiers in Oncology杂志上。

这项回顾性队列研究纳入了2010年至2014年间来自国家癌症数据库(NCDB)的41618例LABC患者。收集了患者的人口学、临床病理、治疗和生存信息。倾向评分(PSM)用于匹配术前放疗患者和术后放疗患者。采用Cox比例风险回归模型分析变量与OS之间的关系。采用Log-rank检验评价各组间OS差异。
共有41618例符合纳入标准,并被纳入初始非匹配分析。在这些患者中,32625例(78.39%)接受术后放疗,8,787例(21.11%)未接受辅助放疗,206例(0.49%)接受术前放疗。与术前接受放疗的患者相比,术后接受放疗的患者更年轻(平均年龄59.24 vs 59.27, p<0.001),更多的亚洲人(p<0.001),更多lumina亚型肿瘤(p<0.001);分化程度较好(p<0.001),肿瘤分期较低(p<0.001),淋巴结分期较高(p=0.005),预后较好(p<0.001);更多的患者接受激素治疗(p<0.001)和BCS (p<0.001)。术前和术后两组在收入、家庭位置、CCI分级、临床分期、化疗和免疫治疗方面的分布无显著差异。
术后放疗的中位随访时间为70.1个月(IQR: 46.85-79.97,范围:2.92-112.95,95%CI: 69.7-70.5),术前放疗的中位随访时间为68.5个月(IQR: 41.13-78.23,范围:4.99-111.57,95%CI: 65.2- 74.8)。术后放疗的LABC患者5年生存率为80.01%(79.56-80.47),术前放疗的患者5年生存率为64.08%(57.55- 71.34)。在未匹配队列的生存分析中,与不放疗患者相比,术后放疗可改善患者OS(p<0.0001)。同样,在多变量Cox分析中,经混合因素调整后,接受术后放疗的患者的死亡率降低了38%[调整后的HR (AHR) =0.62, 95%CI: 0.60-0.65, p<0.001]。然而,术前接受放疗的患者与未接受放疗的患者的预后无显著差异(HR=0.85, 95%CI: 0.68-1.06, p=0.148;AHR=0.88, 95%CI: 0.70-1.11, p=0.282)。

PSM前OS比较
进行PSM后,术后放疗患者的中位随访时间为71.4个月(IQR: 34.37-75.22,范围:4.50-107.04,95%CI: 67.40-75.20),术前放疗患者的中位随访时间为68.5个月(IQR: 65.20-74.80,范围:4.99-111.57,95%CI: 65.2- 74.8)。术后放疗患者的5年生存率为66.29%(59.82-73.47),术前放疗患者的5年生存率为64.08%(57.55-71.34)。
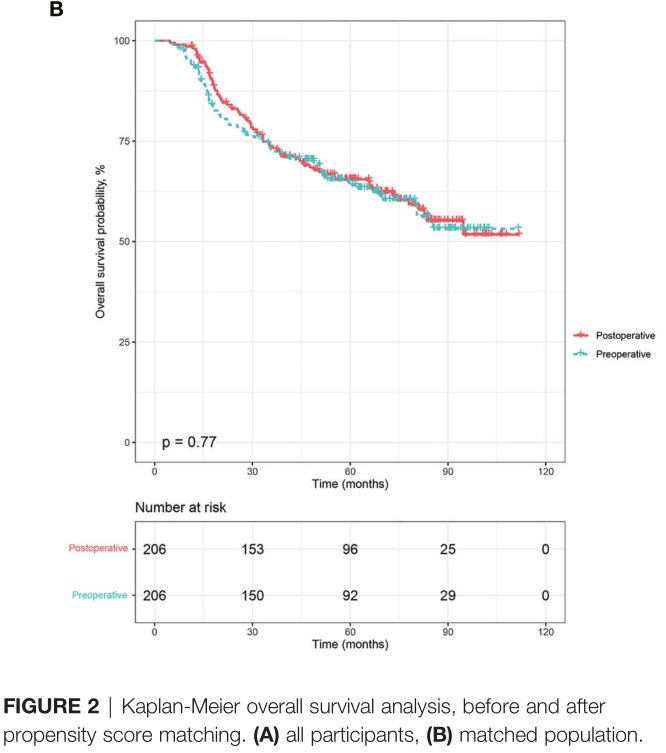
PSM后OS比较
在匹配队列的多变量分析中,≥70岁患者的死亡风险比35-50岁患者高3倍(AHR= 3.83, 95%CI: 1.81-8.11, p<0.001)。黑人患者的OS较白人差 (AHR= 1.59, 95%CI: 1.07-2.37, p<0.001)。此外,在匹配队列中与较差OS相关的因素有:T3 (T3 vs T0-1: AHR = 2.09, 95%CI: 1.09 - -4.02, p = 0.027)和T4 (T4 vs T0-1: AHR = 3.45, 95%CI: 1.82 - -6.54,p<0.001), N1 (N1 vs N0: AHR = 3.37, 95%CI: 1.48 - -7.68, p = 0.004), N2 (N2 vs N0: AHR = 10.01, 95%CI: 4.59 - -21.83,p<0.001),和N3 (N3 vs N0:AHR = 10.26, 95%CI: 4.62-22.78, p<0.001),三阴性型(三阴性型vs Luminal: AHR= 9.02, 95%CI: 3.90-20.86, p<0.001), Her-2阳性型(Her-2阳性vs Luminal: AHR= 4.17, 95%CI: 1.48-11.72, p=0.007),以及接受乳房根治术的患者(AHR= 1.71, 95%CI: 1.10-2.66, p=0.017)。
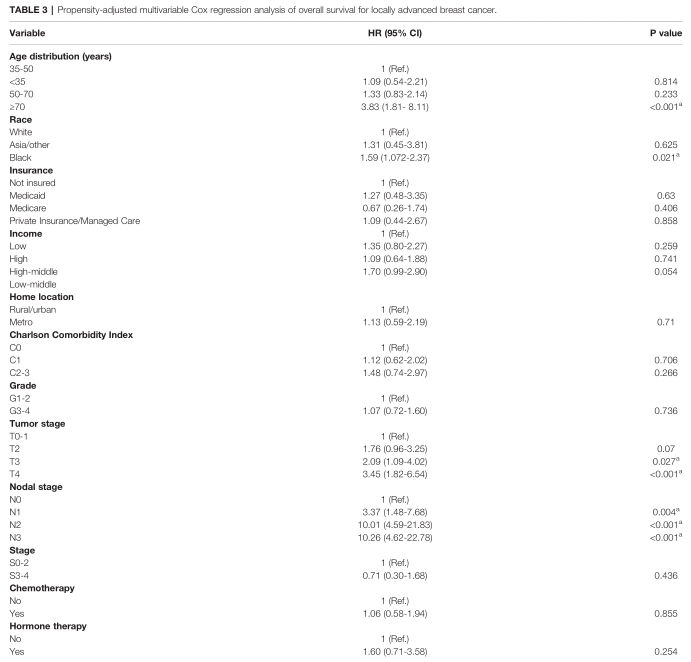
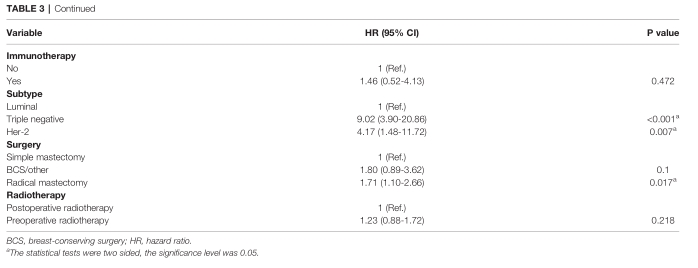
PSM队列多因素分析OS相关因素
最后,术前接受放疗的患者与术后接受放疗的患者预后相似(AHR=1.23, 95%CI: 0.88-1.72, p=0.218)。生存分析显示LABC患者术前放疗与术后放疗OS无差异(p=0.77)。
此外,G0 (HR=1.45, 95%CI: 1.01-2.07, p=0.044)和G1-2亚组(AHR=1.74, 95%CI: 1.59-5.96, p=0.001)术前接受放疗患者的OS比术后接受放疗患者的OS更差。

亚组分析
综上,研究表明,局部晚期乳腺癌(LABC)患者术后放疗可改善患者预后。术前放疗并不能比术后放疗改善患者预后。
原始出处:
Deng Y, Li H, Zheng Y, Zhai Z, Wang M, Lin S, Li Y, Wei B, Xu P, Wu Y, Deng X, Yang S, Lyu J, Hu J, Dong H and Dai Z (2021) Impact of Preoperative vs Postoperative Radiotherapy on Overall Survival of Locally Advanced Breast Cancer Patients. Front. Oncol. 11:779185. doi: 10.3389/fonc.2021.779185
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ABC#
50
#局部晚期#
29
#Oncol#
31
#术后放疗#
36
受教了
51
#局部#
33
很好的文章
55