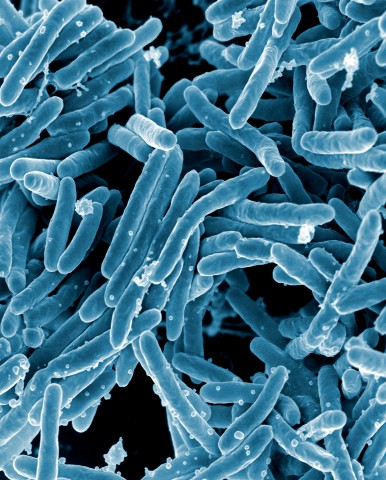
ANN SURG:胃癌Lauren分型是与术后复发有关的重要因素
2017-12-23 MedSci MedSci原创
很少有研究关注西方患者接受根治性胃癌切除术后复发情况。ANN SURG近期发表了一篇文章,研究胃癌患胃食管交界处癌切除后的复发部位。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#术后复发#
30
非常好的文章.学习了
54
非常好.学习了
56
呵呵呵.学习了
53
henhao
64
非常好.谢谢分享
65
谢谢分享
26
学习了新知识
30