常用抗菌药物相互作用表,果断收藏!
2016-12-30 佚名 药圈
1、β-内酰胺类抗菌药物2、氨基糖苷类抗菌药物3、氯霉素4、大环内酯类5、四环素类6、多粘菌素类7、抗结核药8、(去甲)万古霉素9、甲硝唑10、呋喃类11、喹诺酮类12、磺胺药13、抗真菌药
1、β-内酰胺类抗菌药物
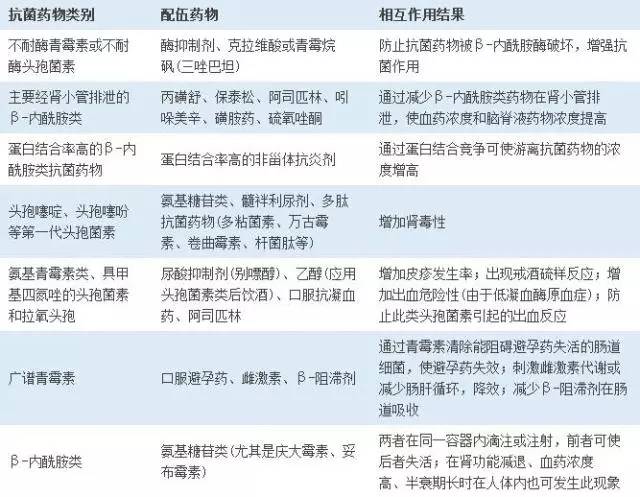

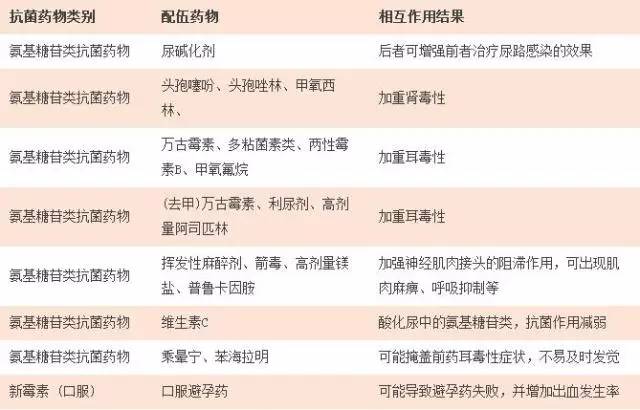
2、氨基糖苷类抗菌药物
3、氯霉素

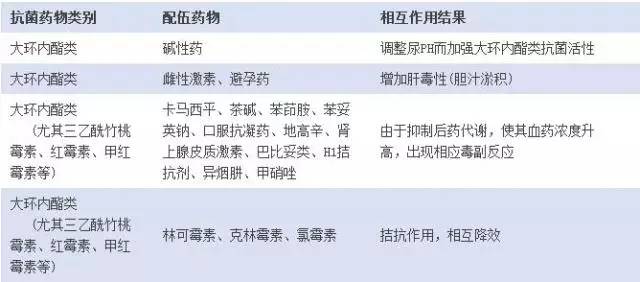
4、大环内酯类
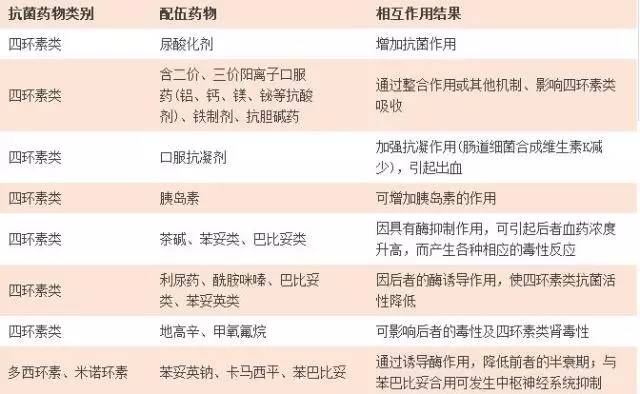
5、四环素类
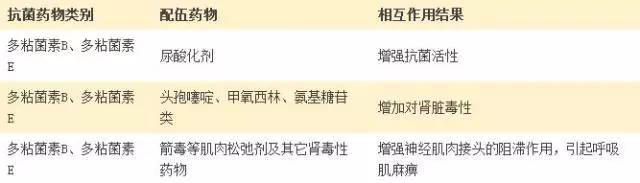
6、多粘菌素类
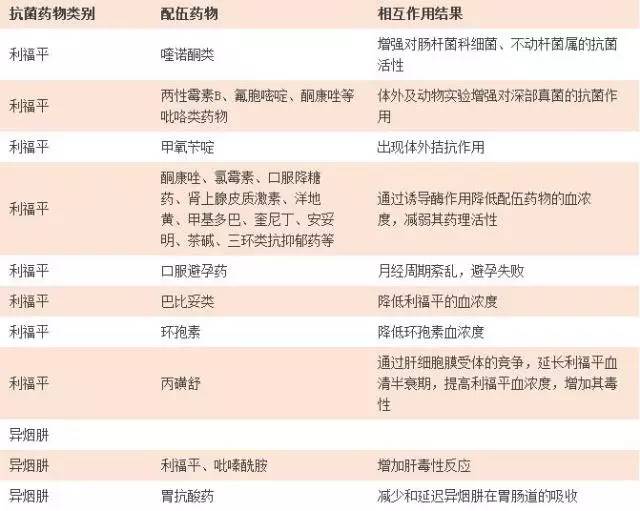
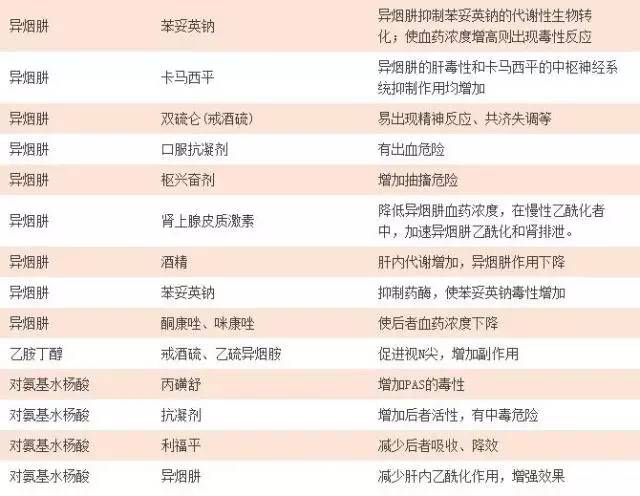
7、抗结核药
8、(去甲)万古霉素

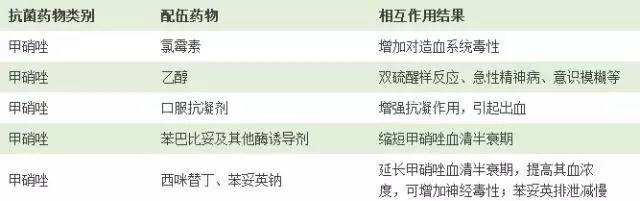
9、甲硝唑
10、呋喃类

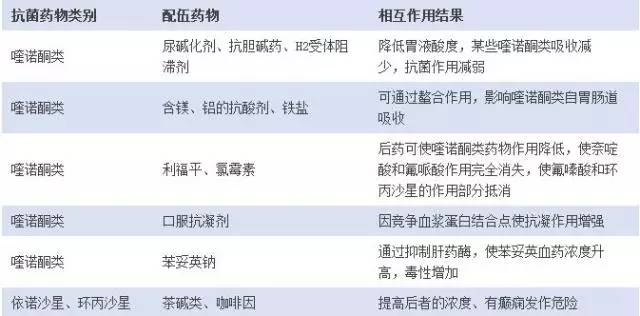
11、喹诺酮类
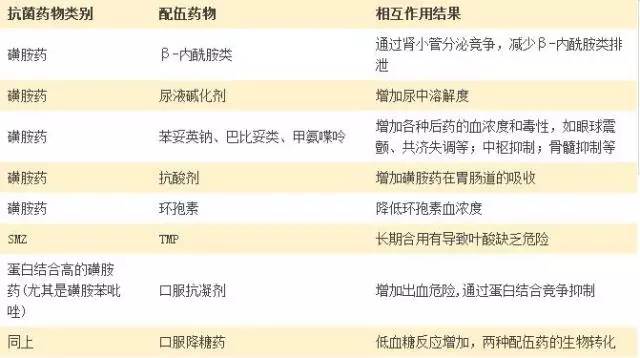
12、磺胺药
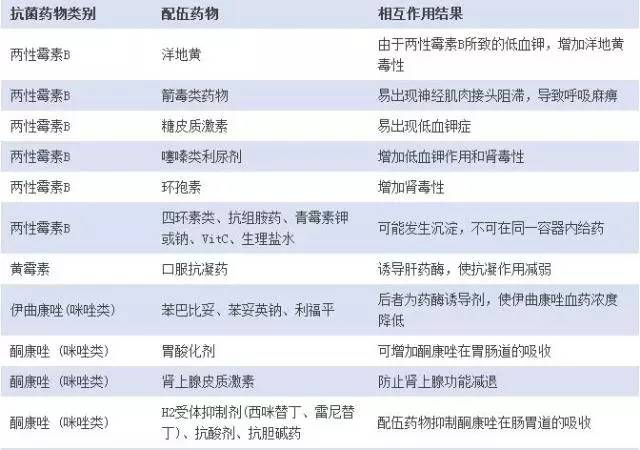
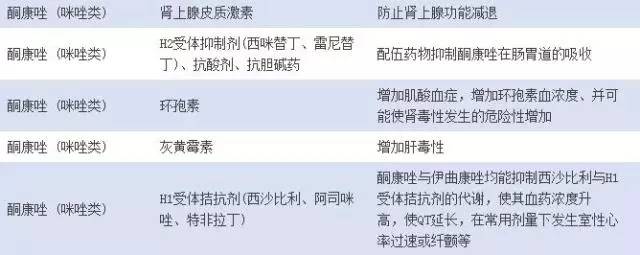
13、抗真菌药
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#相互作用#
35
继续学习中
45
小编辛苦了!为我们整理如此齐全的资料,供学习探究。点赞啦!谢谢!
62
文章不错,值得学习
50
#抗菌#
35
#抗菌药#
32
#互作#
30
#药物相互作用#
33
一目了然,总结的太好了
40
学习了很多先进的医学知识讲座
47