Lancet:PET-CT辅助前列腺癌术后放化疗可有效提高生存率!
2021-05-15 MedSci原创 MedSci原创
将18F-PET/CT纳入前列腺切除术后的放疗决策和计划中,可显著提高无生化复发或持续存在的生存率。
PET/CT,全称“正电子发射断层扫描/X射线计算机断层成像 ”,是筛查全身早期肿瘤的方法。它将PET和CT两个设备有机结合起来,同时具有两者的功能。因其将PET图像与CT图像融合,可以明显提高诊断的准确性、灵敏度及特异性。
Fluciclovine(18 F),是一种诊断剂,可以根据前列腺特异性抗原(PSA)水平升高,用于怀疑患有前列腺癌复发的男性进行PET成像。当PSA轻度升高时,大多数影像学检查均无法定位复发性前列腺癌。但18F标记的PET扫描比CT扫描和 11 C标记的胆碱PET扫描更敏感。
由于传统的CT和骨扫描对于高危前列腺癌患者分期的灵敏度不佳,所以研究人员一直致力于考察PET-CT新成像的效果。去年发表在《柳叶刀》Lancet杂志上的澳大利亚研究发现,前列腺特异性膜抗原(PSMA)可替代常规CT和骨扫描用于高危前列腺癌患者分期。
近日,来自美国埃默里大学温希普癌症研究所放射肿瘤学系的专家进一步研究了与传统骨扫描及CT、MRI相比18F-PET/CT在改善前列腺切除术后挽救性放疗的癌症控制方面的作用,结果再次发表在最新的Lancet杂志上。
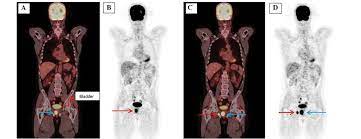
EMPIRE-1是一项单中心、开放标签的2/3期随机对照试验,前列腺癌患者在前列腺切除术后可检测到PSA,且常规影像学检查阴性(无骨盆外或骨发现),按1:1的比例随机分配到仅由常规影像学指导的放疗或常规影像学加18F-PET/CT。计算机生成的随机分配按PSA浓度、不良病理指标和雄性激素剥夺治疗意图进行分层。
在18F-PET/CT组中,放疗决定严格由PET结果决定,PET结果也被用于靶点划定。主要终点是3年无事件生存期(EFS),事件定义为生化或临床复发或进展,或开始系统治疗,对接受放疗的患者进行单变量和多变量分析。
试验流程
2012.09.18-2019.03.04期间,共165名患者被随机分配,中位随访时间为3.52年。总的来说,传统成像组和18F-PET/CT组的中位生存期均未达到预期要求。其中,传统成像组的3年无事件生存率为63.0%(95%CI:49.2-74.0),而18F-PET/CT组为75.5%(95%CI: 62.5-84.6)(差异12.5)。
在调整后的分析中,PET/CT组无事件生存率显著升高(HR=2.04[95% CI:1.06-3.93)。两个研究组的毒性相似,最常见的不良事件是晚期尿频或尿急(常规成像组81名患者中有37人[46%],PET组76人中有31人[41%]),以及急性腹泻(常规成像组有11人[14%],PET组有16人[21%])。

两组患者随访期间无事件生存率
由此可见,将18F-PET/CT纳入前列腺切除术后的放疗决策和计划中,可显著提高无生化复发或持续存在的生存率。在前列腺癌患者的放疗决策和计划中纳入新型PET放射线,值得进一步研究。
参考文献:
18F-fluciclovine-PET/CT imaging versus conventional imaging alone to guide postprostatectomy salvage radiotherapy for prostate cancer (EMPIRE-1): a single centre, open-label, phase 2/3 randomised controlled trial. https://doi.org/10.1016/S0140-6736(21)00581-X
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#PE#
24
#Lancet#
29
#生存率#
40
#放化疗#
29
#PET#
38
#PET-CT#
46
顶刊就是不一样,质量很高,内容精彩!学到很多
54
前列腺癌相关研究,学习了,谢谢梅斯
42