Dev. Cell:Raf-1被认为是新血管形成的关键性蛋白
2012-01-20 MedSci MedSci原创
内皮细胞之间新生的细胞间接触。跨膜蛋白血管内皮细胞钙黏蛋白(VE-cadherin,绿色显示)介导细胞连接的产生,且与细胞内肌动蛋白细胞骨架(红色显示)连接在一起。细胞核染成蓝色。图片来自Reiner Wimmer。 新研究解释了在新血管发育期间内皮细胞如何调节它们之间的结合,并且是第一次证实蛋白Raf-1在决定细胞之间结合强度中发挥着关键性作用。如果Raf-1不存在时,细胞不能够粘附在一起
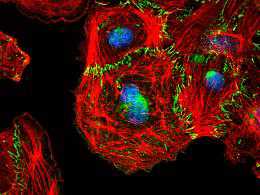
内皮细胞之间新生的细胞间接触。跨膜蛋白血管内皮细胞钙黏蛋白(VE-cadherin,绿色显示)介导细胞连接的产生,且与细胞内肌动蛋白细胞骨架(红色显示)连接在一起。细胞核染成蓝色。图片来自Reiner Wimmer。
新研究解释了在新血管发育期间内皮细胞如何调节它们之间的结合,并且是第一次证实蛋白Raf-1在决定细胞之间结合强度中发挥着关键性作用。如果Raf-1不存在时,细胞不能够粘附在一起,从而抑制新血管形成。这一发现可能有朝一日导致人们开发出治疗癌症的新方法。
芽生式血管生成(angiogenic sprouting),即一种从现有血管长出新血管的过程,是一把双刃剑。它能够让胚胎长出心血管系统,同时对于成年人组织再生也是至关重要的。但是它也给生长中的肿瘤供给营养物和氧气。
血管生成(angiogenesis)是集体性细胞迁移的一个例子。细胞成组移动,并且通过称作黏着接合(adherens junction)的连接保持在一起。如果细胞要想移动,它们不得不持续地建立和破坏这些连接。如果接合太牢固的话,它们肯定不能发生移动,但是如果接合太脆弱的话,这群细胞将分裂开。这种机制是如何控制的,人们之前一直不得而知。
如今,来自奥地利维也纳大学和维也纳医科大学联合创建的马克斯-F-佩鲁茨实验室(Max F. Perutz Laboratories)的研究细胞信号转导的Manuela Baccarini研究小组揭示了这种机制。他们已确定一种多功能信号转导分子Raf-1在这种过程中发挥着关键性的作用。
论文第一作者Reiner Wimmer解释道,“当我们在体外能够对发育中的血管使用视频显微镜(video microscopy)观察时,实际的突破才会取得。我们发现没有Raf-1的细胞一直活跃地迁移,但是只是作为单个细胞进行迁移。它们不能成组迁移。”
这一发现在未来实验中的意义不言而喻:Raf-1的作用是促使新的黏着接合产生,为此它们需要一种激酶以便重构细胞骨架。这意味着Raf-1通过造成细胞骨架的局部重构来微调迁移中细胞之间的结合。
因为芽生式血管生成对于肿瘤长成也是必需的,人们可能有朝一日利用这一新发现开发靶向Raf-1和这种控制机制其他部分的癌症疗法,从而破坏肿瘤生长所需的环境。(生物谷:towersimper编译)
Angiogenic Sprouting Requires the Fine Tuning of Endothelial Cell Cohesion by the Raf-1/Rok-α Complex
Reiner Wimmer, Botond Cseh, Barbara Maier, Karina Scherrer, Manuela Baccarini
Sprouting angiogenesis, crucial for the development of new blood vessels, is a prime example of collective migration in which endothelial cells migrate as a group joined via cadherin-containing adherens junctions (AJ). The actomyosin apparatus is connected to AJ and generates contractile forces, which, depending on their strength and duration, increase or decrease cell cohesion. Thus, appropriate spatiotemporal control of junctional myosin is critical, but the mechanisms underlying it are incompletely understood. We show that Raf-1 is an essential component of this regulatory network and that its ablation impairs endothelial cell cohesion, sprouting, and tumor-induced angiogenesis. Mechanistically, Raf-1 is recruited to VE-cadherin complexes by a mechanism involving the small G protein Rap1 and is required to bring the Rho effector Rok-α to nascent AJs. This Raf-1-mediated fine tuning of Rok-α signaling allows the activation of junctional myosin and the timely maturation of AJ essential for maintaining cell cohesion during sprouting angiogenesis.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Cell#
28
#CEL#
32
#Dev#
28