选择性根管再治疗在磨牙中的应用1例
2019-10-08 乔佳男 杜启涛 全科口腔医学电子杂志
患者男性,50岁,2012年09月26日因“右上后牙牙龈溢脓1年余”于大连市口腔医院就诊,体健,否认系统疾病史和药物过敏史。患者2年前牙疼牙于外院行根管治疗,1年前出现牙龈反复溢脓。口外检查:颜面对称,张口度正常,下颌无偏斜,颞下颌关节无弹响,无压痛,未触及肿大淋巴结。口内检查:16复合树脂充填,叩痛(+),无松动,探诊颊侧粘膜瘘孔。
根管治疗术是目前治疗牙髓病根尖周病最有效的方法,取得了满意的临床效果,由于根管系统复杂性、器械操作局限性及一些医源性因素,初次根管治疗术后总成功率为68%~85%,根管治疗仍有失败的可能。对于失败病例,非手术性根管再治疗术是首选治疗方法,在磨牙根管治疗后疾病中,通过CBCT对病灶精准定位以及根管显微镜入路指导,仅针对引起病灶的根管进行选择性的再治疗即选择性根管再治疗。
1.病例报告
患者男性,50岁,2012年09月26日因“右上后牙牙龈溢脓1年余”于大连市口腔医院就诊,体健,否认系统疾病史和药物过敏史。患者2年前牙疼牙于外院行根管治疗,1年前出现牙龈反复溢脓。口外检查:颜面对称,张口度正常,下颌无偏斜,颞下颌关节无弹响,无压痛,未触及肿大淋巴结。口内检查:16复合树脂充填,叩痛(+),无松动,探诊颊侧粘膜瘘孔。
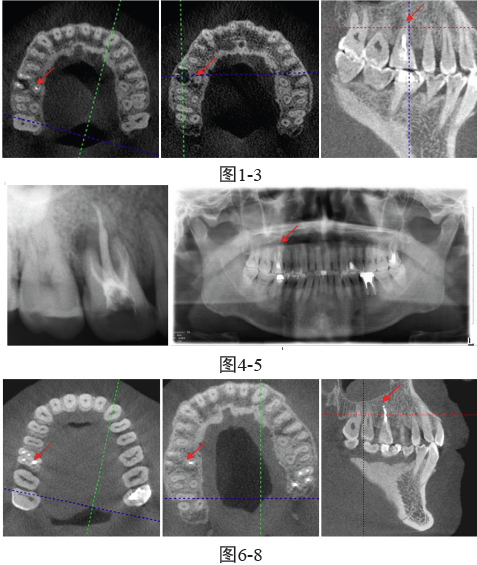
辅助检查:CBCT定位发现虽病变来源是在腭根根尖区根管充填不致密影像,暗影累及颊根(图1-3)。诊断:16腭根残髓炎。治疗:16腭根根管再治疗术治疗过程:1)去除16充填物,打开腭根,去除根管内充填物,根管锉探查腭根根管,探痛,行腭根根管内麻醉,彻底清除腭根根管内残髓、微生物等,冲洗干燥根管,封药。2)一周后复诊,16粘膜瘘孔愈合,叩痛(-),腭根内无明显渗出,行16腭根根管充填术,术后RVG显示腭根充填致密,恰填(图4);四年后复诊:患者症状完全消失,根尖阴影减小,牙周膜间隙正常,硬板完整(图5);6年后复诊:CBCT示腭侧根尖充填致密,腭侧及颊侧根尖阴影消失(图6-8)
2.讨论
2.1根管再治疗病因
根管治疗失败的原因包括根管充填质量不佳30.4%(欠填、超填、不密合);遗漏根管19.7%;冠部封闭不佳。除此之外根管治疗的成功与否与患牙的解剖位置有关,在CBCT指导下,前牙、前磨牙,磨牙的初次根管治疗成功率分别是:91.1%、90.6%,75.5%;对于磨牙来说,根管数目不定(MB2)、下颌第一磨牙远中舌侧根管以及下颌第二磨牙C型根管的近中舌侧根管;根管形态变异如弯曲钙化;而且磨牙位于口腔后方操作空间有限,尤其是上颌磨牙常常颊侧倾斜,所以磨牙根管再治疗研究变得尤为重要。
2.2根管治疗后疾病的治疗方法
根管治疗后疾病(post-treatment endodontic disease,PED)是指根管治疗后患牙的根尖周病变未愈合或出现新的根尖周病变,病理学特征主要表现为根尖周组织的炎症。根管治疗后疾病的治疗方法包括根管再治疗和根尖手术。
2.2.1根管再治疗
根管再治疗的理念是“全或无”即对有临床指症的患牙进行全部再治疗或不治疗。即根管再治疗术通过去除根管内全部的充填物,重新建立根管通道,再次对根管进行彻底预备、消毒并完成严密充填。意义在于清除未控制的感染灶,是保存患牙的经典方法,与首次根管治疗有许多不同之处。旋转镍钛器械的使用提高了根管再治疗的效率,但是会损伤牙本质削弱根管壁并对根管壁产生更大的压力,许多试剂在溶解牙胶的同时也会导致牙本质的软化降低牙本质的强度,增加了根折的可能性。临床医师必须熟悉此类病例的髓室和根管解剖形态,借助手术显微镜,有针对性的寻找髓室和根管口,以免造成髓室底穿或根管侧穿。
2.2.2根尖手术
传统根尖外科手术包括很多术式而现在我们所提及的根尖手术是指显微根尖外科手术的主要内容为根尖切除术和根管倒充填术。根管治疗后疾病手术治疗的适应证:①根管内存在折断器械、根管内台阶、根管不通以及根管原充填物无法去除,不宜使用根管再治疗技术疏通根管的患牙;②根管再治疗后根尖周病变不愈合的患牙;口腔显微镜、超声器械和新材料等应用于根管外科领域使得根尖手术的成功率从44.3%~57%提高到80%~90%。考虑到根尖手术的有创性,患者的身体也必须满足条件。
2.3选择性根管再治疗
2.3.1选择性根管再治疗概念
选择性根管再治疗是根管再治疗治疗术式和根尖手术的选择性相结合的方法即将传统根管再治疗仅运用到通过CBCT或根尖片定位的磨牙病变根管中;此病例术前曲面断层片中病变蔓延整个根尖,但从CBCT最终定位病变为腭侧根管根尖部欠充,颊侧的阴影是腭侧病变累计,最终仅针对腭侧根管进行选择性再治疗,经过6年病例回访,证实选择性根管再治疗的可信性及有效性。在磨牙的根管治疗后疾病中,通过CBCT的对病灶的精准定位以及根管显微镜的入路指导,仅针对引起病灶的根管进行选择性的再治疗,这样既可以减少其他没有问题的根管的过度切削又减轻患者的经济压力,减少操作时间同时避免再治疗过程中意外的发生。刘彦等认为CBCT问世以来,已广泛应用于包括牙体牙髓在内的各个学科,使得根管治疗及再治疗的成功率得以提升,也为选择性根管再治疗提供可能。
2.3.2选择性根管再治疗适应症
根管充填质量不佳:在磨牙根管治疗后疾病中如上颌磨牙腭侧根管及下颌磨牙远中根管较粗大导致根管充填不严密并最终导致患牙出现根管治疗后疾病,在CBCT指导下确定病灶仅针对充填质量不佳根管进行再治疗。遗漏根管:在磨牙根管治疗后疾病中如上颌第一磨牙MB2、下颌前牙前磨牙双根管、下颌第一磨牙远中舌侧根管、下颌第二磨牙C型根管、上颌磨牙腭侧双根管等常常被遗漏,而其余根管治疗并没有问题,在CBCT指导下确定病灶仅针对遗漏根管进行再治疗。
3.结论
在微创理念的指导下,对于磨牙的根管治疗后疾病来说,选择性根管再治疗绝对会为临床医生提供更好的选择。但是选择性根管再治疗是有条件的,除了严格把握适应症以外,对于临床医师的技术水平,器械的配置以及材料的选择都有很高的要求。选择性根管再治疗还需要更多实践检验,希望在微创与清创并不矛盾的前提下,能够花费更少的时间和精力为患者解决问题,做到有的放矢,精准微创。
原始出处:
乔佳男,杜启涛.选择性根管再治疗在磨牙中的应用1例病例报告及6年回访[J].全科口腔医学电子杂志,2018,5(28):91-93.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#根管再治疗#
37
#选择性#
35
#根管#
27
#再治疗#
44
#磨牙#
23