Cell Stem Cell:开发出在体外长期培养成体干细胞的方法
2016-06-18 佚名 生物谷
在一项新的研究中,来自美国麻省总医院(MGH)等机构的研究人员开发出的一种新方法可能引发成体干细胞培养领域变革。研究人员描述了获得来自在日常治疗肺部疾病期间收集的各种组织样品中的气道干细胞(airway stem cell),并对它们进行增殖。这种方法似乎也可用于几种其他的组织,如皮肤、胃肠道内壁和生殖道。相关研究结果于2016年6月16日在线发表在Cell Stem Cell期刊上,论文标

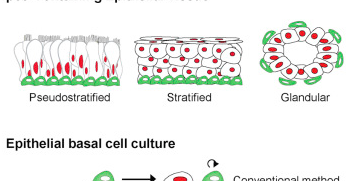
在一项新的研究中,来自美国麻省总医院(MGH)等机构的研究人员开发出的一种新方法可能引发成体干细胞培养领域变革。研究人员描述了获得来自在日常治疗肺部疾病期间收集的各种组织样品中的气道干细胞(airway stem cell),并对它们进行增殖。这种方法似乎也可用于几种其他的组织,如皮肤、胃肠道内壁和生殖道。相关研究结果于2016年6月16日在线发表在Cell Stem Cell期刊上,论文标题为“Dual SMAD Signaling Inhibition Enables Long-Term Expansion of Diverse Epithelial Basal Cells”。
“这种新方法为研究哮喘或慢性阻塞性肺病(chronic obstructive pulmonary disease, COPD)等任何一种气道疾病开辟了新途径”,论文通信作者、MGH再生医学中心科学家、哈佛医学院医学副教授Jayaraj Rajagopal博士说,“尽管我们在过去仅能够允许成体干细胞增殖几代,但是如今我们能够在多家实验室持续几年培养出足够多的成体干细胞用于实验。我们的方法也是非常简单的,避免了之前培养系统的复杂性,使得很多实验室更容易采用它。”
人们已提出很多假设来解释在体外培养时只能有限地维持成体干细胞的性能,包括保护染色体末端的端粒丢失和细胞衰老。Rajagopal团队着重关注一种已知调节细胞生长和关键性分化过程的细胞信号通路。当被TGF-β和骨形态发生蛋白(BMP)等蛋白激活时,这种信号通路利用胞内蛋白SMAD将信号传递到细胞核。
在这项研究中,研究人员研究了抑制SMAD通路是否能够通过阻断体外培养的成体干细胞分化而促进它们增殖。在一系列实验中,他们首先证实TGF-β/BMP和SMAD信号通路在已分化的细胞中是有活性的,但在成体干细胞中是没有活性的。在发现阻断SMAD信号通路能够阻断小鼠气道干细胞分化后,他们发现同时阻断TGF-β/BMP和SMAD信号通路允许气道干细胞增殖很多代。他们能够从支气管镜检(bronchoscopy)时采集的样品中获得人气道干细胞。引人注目的是,他们也成功地从一些痰液样品---咳嗽时从呼吸道排除的液体---中获得人气道干细胞并对它们进行维持。
研究人员发现这一方法也可用于很多组织,包括皮肤、食道和乳腺等。这些器官中有不少当前还不能在体外培养,因此,还有待观察这些领域的科学家们是否能够培养来自利用其它侵入性最小的方法(如收集分泌物)获得的样品中的干细胞。如果经证实确实能够的话,那么它代表着个人化疾病研究方法取得重大进展。
原始出处
Hongmei Mou, Vladimir Vinarsky, Purushothama Rao Tata, Karissa Brazauskas, Soon H. Choi, Adrianne K. Crooke, Bing Zhang, George M. Solomon, Brett Turner, Hermann Bihler, Jan Harrington, Allen Lapey, Colleen Channick, Colleen Keyes, Adam Freund, Steven Artandi, Martin Mense, Steven Rowe, John F. Engelhardt, Ya-Chieh Hsu, Jayaraj Rajagopal.Dual SMAD Signaling Inhibition Enables Long-Term Expansion of Diverse Epithelial Basal Cells.Cell Stem Cell.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
23
#成体干细胞#
34
#Cell#
26
#stem cell#
35
#STEM#
25
值得借鉴
137
可以推广
113
好文章,值得学习
179