 在卒中发生后4.5小时内用阿替普酶进行静脉溶栓(IVT)是急性缺血性卒中(AIS)的一种循证药物治疗。
在卒中发生后4.5小时内用阿替普酶进行静脉溶栓(IVT)是急性缺血性卒中(AIS)的一种循证药物治疗。
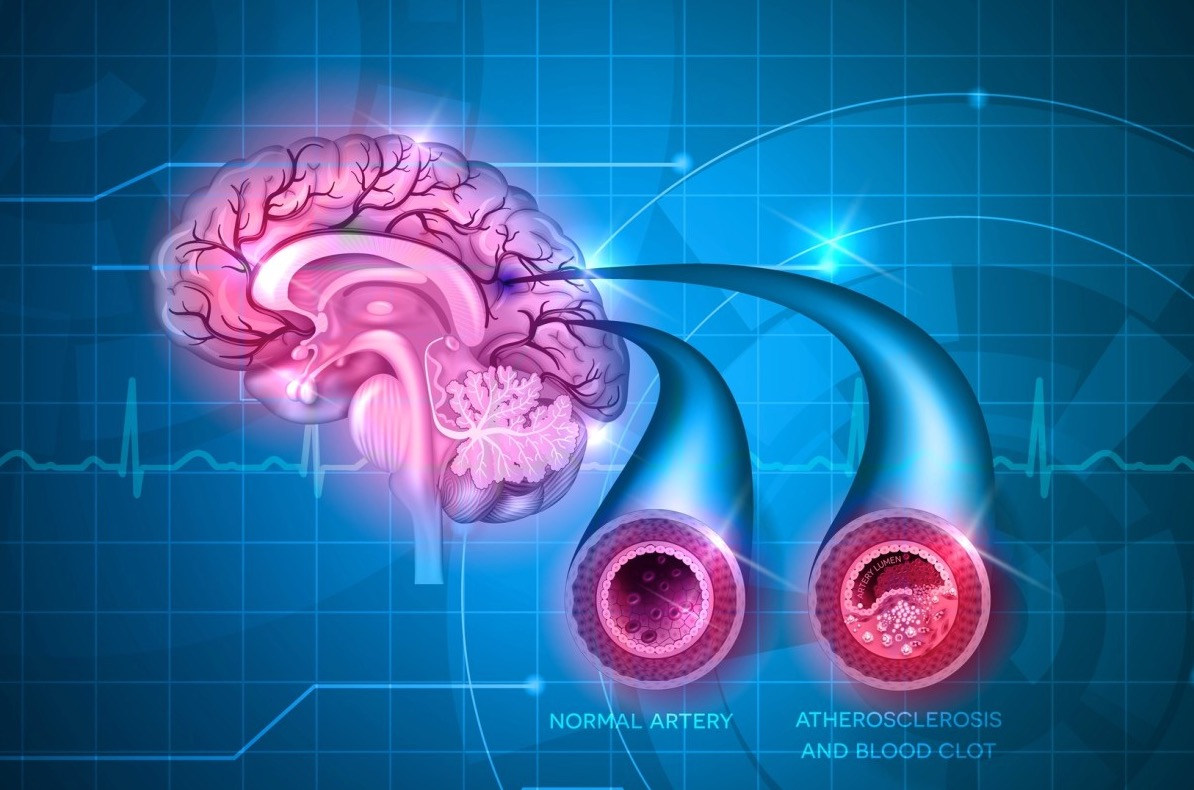
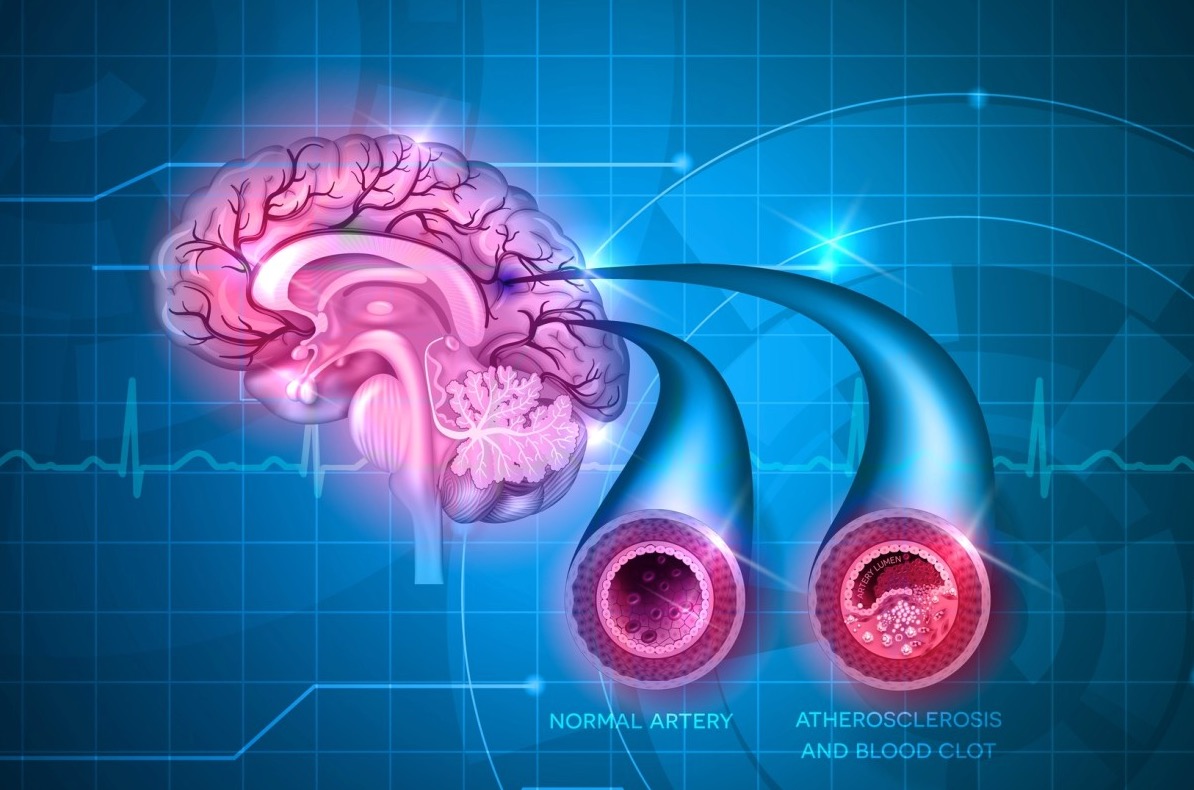
然而,中风后的结果与最初的中风严重程度和血管闭塞的位置密切相关,虽然IVT对严重的中风有好处,但大动脉闭塞(LAO)的再通率很低。随机对照试验(RCTs)表明,在前循环LAO中风中,在标准护理(包括IVT)的基础上增加血管内血栓切除术(EVT)比单纯药物治疗有好处。
两项荟萃分析证实,血栓切除术可使动脉再通率高,并可显著改善3个月后的功能预后,且死亡率不增加。有研究报告称,与单纯EVT相比,接受EVT的患者IVT治疗的安全性和有效性存在矛盾。IVT治疗可能会延长启动EVT的时间,增加出血性并发症的风险。相反,IVT可能对多灶性缺血或合并远端闭塞有益,增加再通的成功率,甚至可以裂解血栓,避免EVT的需要。
最近中国的两项RCT显示直接EVT与IVT联合治疗相比非劣势,而日本的一项RCT没有显示非劣势。 同时,最近一项对30项研究的荟萃分析显示,与单纯EVT相比,接受EVT+IVT的患者获得了明显更好的功能结果,在倾向性评分匹配后,这种关联仍然显著。
目的。为了验证在血管内血栓切除术(EVT)之前进行静脉溶栓(IVT)治疗与前循环大动脉闭塞(LAO)卒中患者更好的预后有关的假设,我们研究了一个大型的真实世界数据库,即SITS-国际卒中血栓切除术登记册(SITS-ISTR)。
藉此,瑞典卡洛琳斯卡大学的Niaz Ahmed等人,SITS-ISTR中确定了连续记录10名患者的中心,在2014-19年期间,至少有70%的修正Rankin量表(mRS)评分可用。我们将LAO定义为颅内颈动脉、大脑中动脉的第一和第二段以及大脑前动脉的第一段。
主要临床结局是功能独立(mRS 0-2)和3个月后的死亡,以及根据修改后的SITS-MOST,症状性颅内出血(SICH)。并进行了倾向性评分匹配(PSM)和多变量逻辑回归分析。
在42个中心的6350名患者中,3944名(62.1%)接受了IVT治疗。接受IVT+EVT治疗的患者较少出现心房颤动、持续抗凝、既往中风、心力衰竭和中风前残疾。
PSM(propensity score matched)分析显示,IVT+EVT患者的功能独立率高于单纯EVT患者(46.4% vs. 40.3%,P<0.001),3个月时的死亡率较低(20.3% vs. 23.3%,P=0.035)。
两组的SICH率(3.5% vs. 3.0%, p= 0.42)相似。多变量调整的结果与PSM一致。
这个多中心的研究表明,IVT预处理与EVT治疗的LAO卒中的有利结果有关。这些发现虽然对国际常规临床实践有指导意义,但由于观察性设计、未测量的混杂因素和可能存在的适应症的残留混杂因素而受到限制。该研究提供了II级证据,表明与单纯EVT相比,EVT前的IVT可增加3个月后功能独立的概率。
原文出处:
Safety and Outcomes of Thrombectomy in Ischemic Stroke With vs Without Intravenous Thrombolysis
Niaz Ahmed, Michael Mazya, Ana Paiva Nunes, Tiago Moreira, et al.
Neurology Jun 2021, 10.1212/WNL.0000000000012327; DOI: 10.1212/WNL.0000000000012327
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#大血管#
40
#Neurol#
27
#静脉#
35
#取栓#
39
中风是俗称,应该称为缺血性卒中吧
60