J Am Soc Nephrol:同种异体肾移植微血管排斥反应的缺失:一项基于人群的研究
2021-08-20 AlexYang MedSci原创
尽管宿主免疫系统的潜在排斥反应仍然是改善同种异体移植结果的重要障碍,但
尽管宿主免疫系统的潜在排斥反应仍然是改善同种异体移植结果的重要障碍,但肾脏移植仍旧是治疗终末期肾衰竭最经济有效的方法。目前使用的免疫抑制药物已经证明了其在预防和治疗T细胞介导的排斥反应(TMCR)方面的价值。然而,在过去的几十年里,随着急性TMCR的重要性在发病率和功能效果方面都有所下降,抗体介导的排斥反应(ABMR)显然应该视为一种独特的排斥表征,且对移植物的寿命有重要影响。
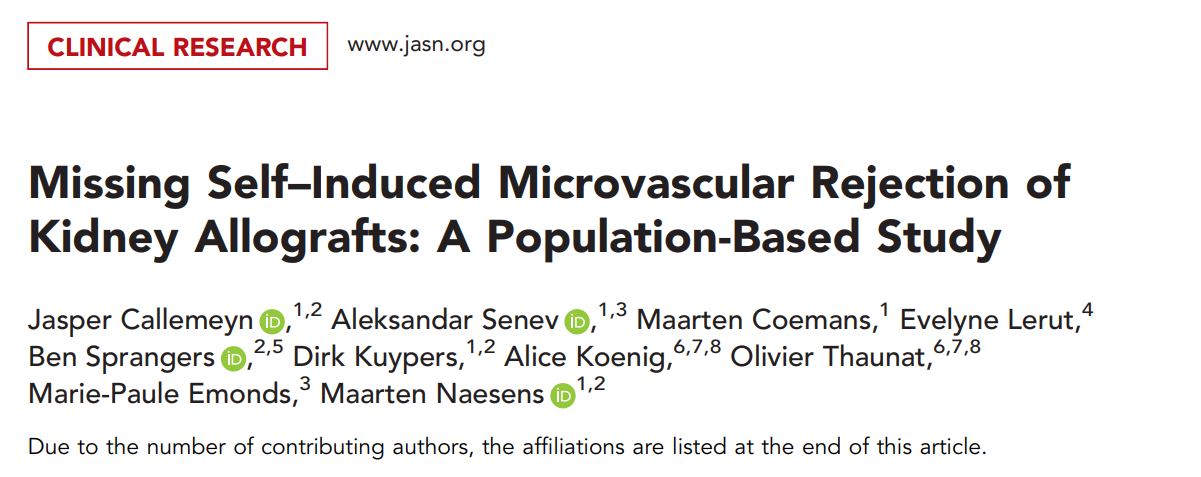
循环的抗HLA供体特异性抗体(HLA-DSA)在患有微血管炎症(MVI)的肾移植受体中经常缺失。Missing self是指供体内皮细胞无法向受体自然杀伤细胞上的抑制性杀伤细胞Ig样受体(KIRs)提供HLA I介导的信号,后果可在体外引起内皮细胞损伤,并与HLA-DSA阴性MVI有关。然而,Missing self作为异体移植排斥的非体液性触发因素的临床重要性仍不清楚。
近期,来自比利时鲁汶大学的研究者在《J Am Soc Nephrol》杂志上发表重要文章,就Missing self作为异体移植排斥的非体液性触发因素的临床重要性进行了一项基于人群的研究。
在2004年3月至2013年2月期间,研究人员对924例连续的肾脏移植进行了一项基于人口的研究,他们对参与者进行了高分辨率的供体和受体HLA分型和受体KIR基因分型。Missing self的定义是没有A3/A11、Bw4、C1或C2的供体基因型,而存在相应的受体抑制性KIR基因。
研究结果发现,在924例移植手术中,研究人员发现399例存在Missing self。Missing self类型的共同出现对增加MVI风险有叠加效应,且两个同时出现的类型存在阈值(风险比[HR],1.78;95%置信区间[95%CI],1.26至2.53),独立于HLA-DSA(HR,5.65;95%CI,4.01至7.96)。另外,Missing self和细胞排斥的病变没有关系。在222名患有MVI的参与者中,有146名没有检测到HLA-DSA;146人中有28人至少有两种Missing self类型。尽管同种异体移植的生存率比HLA-DSA相关的MVI要好,Missing self与MVI后的移植肾小球病变有关(HR,2.51;95%CI,1.12至5.62)。
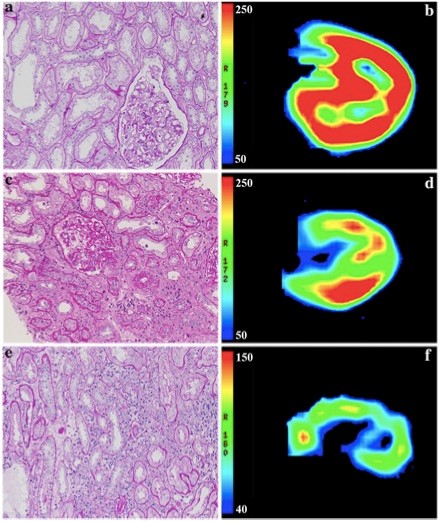
Missing self类型累积与MVI风险有关
综上所述,Missing self会特异和累积地增加肾脏移植后的MVI风险,且与HLA-DSA无关。对Missing self的系统性评估可提高对HLA-DSA阴性MVI的理解,并可能改善诊断分类和病人的风险分层。
原始出处:
Jasper Callemeyn , Aleksandar Senev , Maarten Coemans et al. Missing Self-Induced Microvascular Rejection of Kidney Allografts: A Population-Based Study. J Am Soc Nephrol. Aug 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#同种异体#
48
#排斥#
44
#微血管#
37
#排斥反应#
54