J Dent Res:糖尿病与骨坏死之间的那些事儿
2015-04-18 MedSci MedSci原创
20世纪初期,Marx 和Ruggiero团队首次报道了颌面部静脉注射双磷酸盐类(BPs)造成伤口未愈合骨暴露的案例。大量的研究表明颌骨骨坏死(MRONJ)与药物的使用有关,主要与BP有关。在抗骨吸收患者中,骨坏死的累积发病率达0.7%至18%。最近的抗骨吸收治疗,包括抑制核因子-κB受体活化因子及其配体以及抗血管生成疗法,这些都与MRONJ发生率的升高有关。BP以及其他的抗骨吸收治疗被认为是MR
20世纪初期,Marx 和Ruggiero团队首次报道了颌面部静脉注射双磷酸盐类(BPs)造成伤口未愈合骨暴露的案例。大量的研究表明颌骨骨坏死(MRONJ)与药物的使用有关,主要与BP有关。在抗骨吸收患者中,骨坏死的累积发病率达0.7%至18%。最近的抗骨吸收治疗,包括抑制核因子-κB受体活化因子及其配体以及抗血管生成疗法,这些都与MRONJ发生率的升高有关。
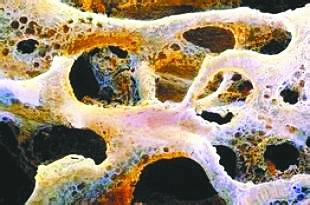
BP以及其他的抗骨吸收治疗被认为是MRONJ发生的高危因素,相关的全身因素包括癌症,年龄,化疗治疗(抗血管生成疗法),相关的并发因素(营养不良,肥胖,贫血,透析),生活方式(酒精,烟草)和药物治疗,如糖皮质激素的应用。疾病相关的局部危险因素包括口腔疾病,口腔卫生不良,以及主要的口腔治疗程序。MRONJ损害骨修复的潜在机制是,抑制破骨细胞活性,感染和炎症,妨碍血管生成或血管的修复。
本研究论述了糖尿病(DM)在MRONJ发病机制中的所起的作用,DM可能会增加骨坏死的风险。
药物相关性骨坏死(MRONJ)是一个严重的并发症,其确切的发病机制尚未清楚。越来越多的证据表明DM是MRONJ发生的重要危险因素,然而,其确切的发病机制同样未完全清楚。DM的治疗及发病机制可能会通过多种途径加剧骨的破坏,包括微血管缺血,内皮细胞功能障碍,降低骨的重塑性以及增加成骨细胞和骨细胞的凋亡等。
总之,DM可诱导免疫细胞功能改变和促进炎症的发生。这增加了癌症治疗过程中慢性感染的风险,同样增加了抗骨吸收药物暴露的风险,从而提高了MRONJ发生的危险。MRONJ具有遗传倾向,加之 CYP 450基因的突变可影响DM治疗药物(如噻唑烷二酮类药物)的降解,可进一步提高MRONJ发生的危险。
Peer A, Khamaisi M.Diabetes as a risk factor for medication-related osteonecrosis of the jaw.J Dent Res. 2015 Feb;94(2):252-60. doi: 10.1177/0022034514560768. Epub 2014 Dec 4.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








好文章,还会关注
50
#骨坏死#
35
学习了,很好
93
从不同角度思考
119
#坏死#
30