眼底血管造影剂致尿总蛋白定量检测结果异常一例
2018-04-28 邵文琦 吴炯 吴卫云 检验医学
患者女,58岁。因“3个月前无明显诱因出现视物模糊,无复视,视力下降”来复旦大学附属中山医院就诊。
【一般资料】
患者女,58岁。
【主诉】
因“3个月前无明显诱因出现视物模糊,无复视,视力下降”来复旦大学附属中山医院就诊。
【现病史】
【体格检查】
体温36.5℃,心率80次/min,呼吸20次/min,血压19.95/11.97kPa。眼压:右眼2.46kPa(18.5mmHg)、左眼2.00kPa(15.0mmHg)。
【辅助检查】
血管B超提示双侧颈动脉粥样硬化。肌电图提示右侧正中神经、腓总神经神经传导速度减慢且波形离散。
【初步诊断】

【治疗】
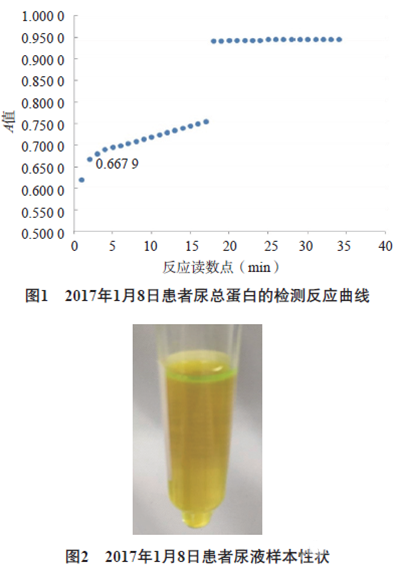
临床拟对患者进一步行眼底激光治疗,因此于2017年1月7日对患者行FFA。检查显示:视乳头阴性,视网膜见散在出血及渗出,累及黄斑,右眼为甚。FFA诊断:双眼重度非增殖性糖尿病视网膜病变,黄斑水肿。2017年1月8日复查24h尿总蛋白定量结果,与1月6日的检测结果相对偏差高达557.89%,24h尿总蛋白定量结果相对偏差高达500.00%。见表1。2.结果分析分析2017年1月8日尿总蛋白项目的检测反应曲线,样本加入后反应吸光度(A)值即刻达到0.6679,见图1。患者样本性状呈明显的荧光黄色,见图2。尿总蛋白试剂为原装配套试剂,结合病史考虑该样本为眼底荧光造影剂对检测方法产生干扰,联系临床,1月8日的尿总蛋白和24h尿总蛋白定量结果报告为污染。3.复查结果2017年1月11日复查24h尿总蛋白定量结果,尿总蛋白为0.10g/L,尿白蛋白为10.0mg/L,24h尿总蛋白定量为0.17g/24h,24h尿白蛋白为17.0mg/24h,与1月6日检验结果相符。
【讨论】
尿液总蛋白的测定有着悠久的历史,常用于肾病、糖尿病或妊娠高血压等疾病的诊断和治疗监测。本实验室使用的尿液/脑脊液总蛋白检测试剂盒采用苄索氯铵作为表面活性剂,在碱性环境下与蛋白质形成稳定、均匀的浊度。苄索氯铵与尿液蛋白质反应产物的吸收峰在505nm处。复旦大学附属中山医院使用的眼底血管造影剂为荧光素钠注射液,其最大吸收波长为493.5nm,在酸性条件下荧光特性会消失,在碱性条件下又会出现。BLOOM等和KOUMANTAKIS等分别报道了荧光素钠对检验项目的干扰情况,荧光素钠在碱性环境下会干扰苄索氯铵方法,造成假阳性结果。鉴于荧光素钠一般在行FFA检查后24~36h排出体外,故建议此类患者可于FFA检查36h后留取尿液标本检测总蛋白。药物干扰是检验项目干扰的重要来源。厂商说明书中往往会列举目前已知的干扰检测方法的药物,但如何识别未知药物的干扰,发现异常的检验报告依然是一线检验工作者面临的重大挑战。因此,“多次结果比较”、“不同项目间的逻辑关系”等审核报告的方法往往是识别此类异常报告的主要方法。尿总蛋白及尿白蛋白存在较大的生物变异度,个体内变异分别为35.5%和36.0%。若短时间内相同项目的结果超过个体内变异,则需警惕异常结果的出现。本例患者3d内连续2次尿总蛋白检测结果的相对偏差达557.89%,24h尿总蛋白定量结果的相对偏差达500.00%,远超正常的生物学变异,应引起报告审核人员的重视。体内总蛋白最主要的组成成分是白蛋白,一般占70%左右。本例患者尿总蛋白浓度急速上升而尿白蛋白水平正常,也应引起报告审核人员的重视。由此可见,从临床意义接近的不同项目之间的逻辑关系能有效发现异常检验报告。临床实验室工作人员应结合患者病情对检测结果进行综合分析及判断,以免影响报告的准确性,进而影响下一步的诊断和治疗。
原始出处:
邵文琦, 吴炯, 吴卫云, 等. 眼底血管造影剂致尿总蛋白定量检测结果异常一例报道[J]. 检验医学, 2018,33(2): 185-187
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#检测结果#
34
#造影#
24
学习了谢谢分享!!
74
好知识值得拥有的
63