JACC Heart Fail:西格列汀或增心衰住院风险
2014-07-10 高晓方 译 医学论坛网
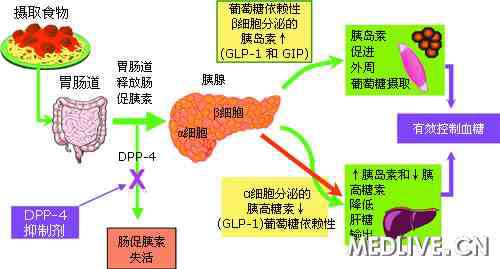
加拿大一项研究表明,在初始伴有心衰的糖尿病患者中,DPP-4抑制剂西格列汀可升高心衰住院风险。 此项研究共纳入7620例接受二甲双胍或磺酰脲治疗且伴有心衰的糖尿病患者,其中887例在诊断心衰后启用西格列汀。主要终点为全因住院或死亡,次要终点为心衰住院、全因死亡或全因住院。中位随访时间为1.4年。 结果显示,在未校正分析中西格列汀应用和未应用者的主要终点和次要终点均无显著差异
加拿大一项研究表明,在初始伴有心衰的糖尿病患者中,DPP-4抑制剂西格列汀可升高心衰住院风险。
此项研究共纳入7620例接受二甲双胍或磺酰脲治疗且伴有心衰的糖尿病患者,其中887例在诊断心衰后启用西格列汀。主要终点为全因住院或死亡,次要终点为心衰住院、全因死亡或全因住院。中位随访时间为1.4年。
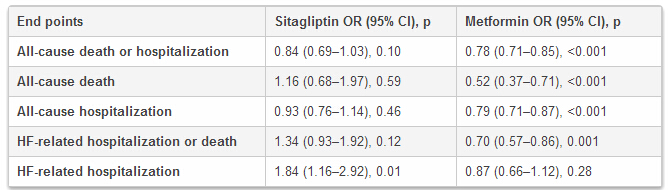
结果显示,在未校正分析中西格列汀应用和未应用者的主要终点和次要终点均无显著差异,但西格列汀应用者的心衰住院率显著升高(比值比[OR] 1.84;P=0.01)。西格列汀导致新发心衰住院风险升高84%,造成伤害所需治疗人数为29。此外,二甲双胍治疗与主要终点相对风险降低22%相关,磺脲类和胰岛素应用者的主要终点风险则分别升高10%和16%。
研究者表示,西格列汀所致的心衰住院风险升高可能具有临床意义,并且对心衰患者选择附加糖尿病治疗药物可能具有指导价值。鉴于DPP-4抑制剂心衰风险临床研究结果并不一致,因此未来需进一步明确西格列汀的风险及获益特征。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JACC#
26
#心衰住院#
51
#住院风险#
40
#ACC#
37
#ART#
27
#HEART#
29