Front Oncol:远端输尿管尿路上皮癌(UC)部分输尿管切除术+辅助放疗的疗效
2021-10-04 yd2015 MedSci原创
该研究表明,对于T3或G3输尿管远端尿路上皮癌患者,与单纯输尿管部分切除术相比,辅助放疗可显著延长无复发生存期。但是PU+ART与根治性肾输尿管切除术的生存率无显著差异。
远端输尿管尿路上皮癌(UC)的金标准治疗是根治性肾输尿管切除术(RNU)和膀胱袖移除。但部分输尿管切除术(PU)也是一种可行的选择,特别是在孤立肾或双侧输尿管癌或慢性肾功能不全的患者。有meta分析结果显示,Ta/T1和G1-G2肿瘤患者在PU和RNU术后的肿瘤特异性生存期(cancer specific survival, CSS)无显著差异。对于T3或G3的患者,PU与RNU相比无复发生存(RFS)、膀胱复发和总生存(OS)更差。而目前辅助放疗(ART)治疗在RNU术后UC的价值仍存在争议。亚洲国家的一些研究表明,RNU术后辅助放疗可改善高危病理因素(T3、G3)患者的LRFS、远处无转移生存(DMFS)或OS。对于PU后伴有G3、T3等不良因素患者,术后放疗是否能提高生存率值得探讨。因此,来自北京大学第一医院的团队开展了回顾性研究,评估T3或G3输尿管远端尿路上皮癌(DUUC)行输尿管部分切除术(PU)后辅助放疗(ART)的预后价值。相关结果发表在Frontiers in Oncology杂志上。
研究分析了2008年1月至2019年9月该院共221例T3或G3患者接受PU或RNU的临床资料。其中PU+ART治疗17例,单纯PU治疗72例,肾输尿管根治术(RNU)132例。评估其临床病理结果。生存率采用Kaplan-Meier法进行评估。Cox回归分析无复发生存期(RFS)、无转移生存期(MFS)、肿瘤特异性生存期(CSS)和总生存期(OS)。
患者中位年龄68岁(IQR 62 ~ 76),中位随访时间43个月(IQR 28 ~ 67)。PU+ART组的切缘阳性率高于单纯PU组(p= 0.026)和RNU组(p= 0.012)。PU+ART组的淋巴结转移明显高于单纯PU组(p= 0.034)。

临床特征
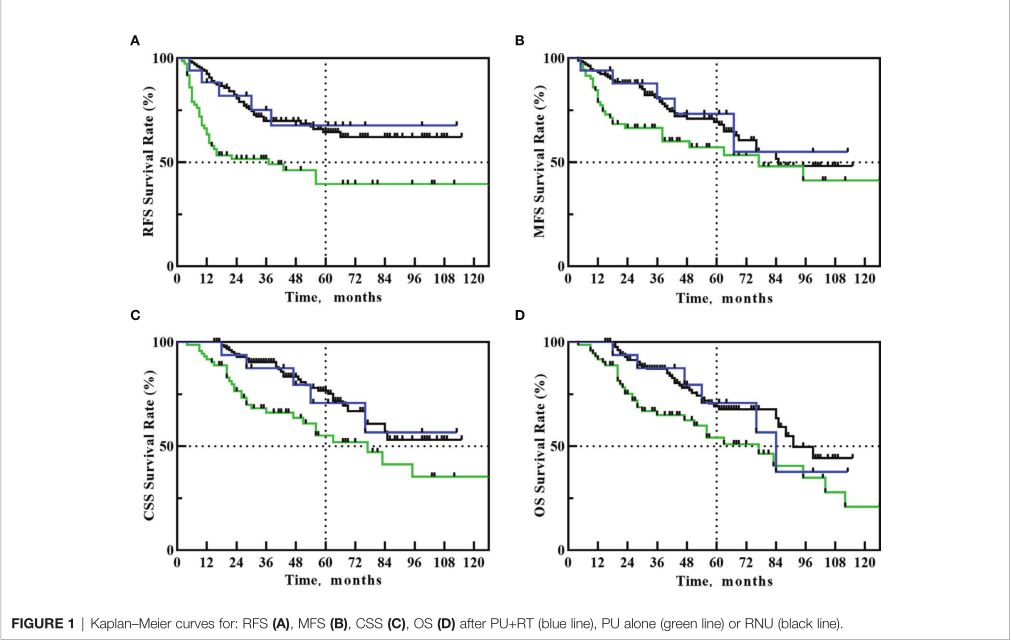
PU+ART组5年RFS、MFS、CSS和OS率分别为67.6%、73.2%、70.7%和70.7%。单纯PU组5年RFS、MFS、CSS和OS率分别为39.5%、57.2%、55.1%和54.1%。RNU组5年RFS、MFS、CSS和OS率分别为64.4%、69.4%、76.6%和69.2%。
预后
与单纯PU组相比,PU+ART显著改善患者5年RFS率 (67.6% vs. 39.5%, HR: 2.431, 95%CI 1.210-4.883, p=0.039)。然而,PU+ART组与RNU组5年RFS差异无统计学意义(67.6% vs. 64.4%, HR=1.113, 95%CI 0.457-2.712, p=0.821)。与单纯PU组比较,PU+ART组5年MFS (73.2% vs. 57.2%, p=0.144)、CSS (70.7% vs. 55.1%, p=0.131)、OS (70.7% vs. 54.1%, p=0.121)差异无统计学意义。与RNU组相比,PU+ART组5年MFS (73.2% vs. 69.4%, p=0.778)、CSS (70.7% vs. 76.6%, p=0.907)和OS (70.7% vs. 69.2%, p=0.985)相似。
因为生存结局的差异仅存在于PU+ART组和PU组的RFS中。为探讨PU术后辅助放疗的疗效。在89例PU患者中,局部复发相关因素进行单变量和多变量分析。肿瘤直径>2.5cm、pN+、G3、手术切缘阳性和非ART均与PU患者局部复发增加显著相关(p<0.05)。在多变量分析中,只有pN+ (HR= 1.625;95% CI 1.063-2.372, p=0.031),非ART (HR =2.590;95% CI 1.855- 3.636, P = 0.016)仍然是局部复发增加的独立预测因素。
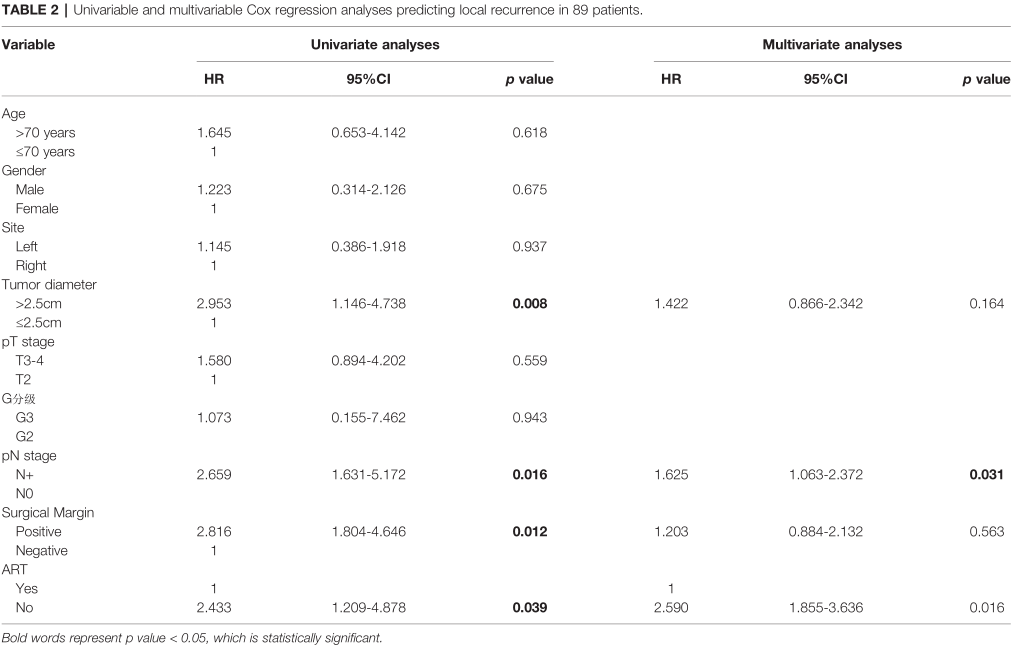
单变量和多变量分析
综上,该研究表明,对于T3或G3输尿管远端尿路上皮癌患者,与单纯输尿管部分切除术相比,辅助放疗可显著延长无复发生存期。但是PU+ART与根治性肾输尿管切除术的生存率无显著差异。
原始出处:
Li H-z, Li X, Gao X-s, Qi X, Ma M-W and Qin S (2021) Oncological Outcomes of Adjuvant Radiotherapy for Partial Ureterectomy in Distal Ureteral Urothelial Carcinoma Patients. Front. Oncol. 11:699210. doi: 10.3389/fonc.2021.699210
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#切除术#
28
#Oncol#
34
#输尿管#
51
#上皮癌#
41
#辅助放疗#
44