Stroke:脑血栓取出后24小时NIHSS评分,可有效预测长期功能
2021-08-18 Freeman MedSci原创
经基线调整后的24小时NIHSS,是预测血管内治疗患者90天mRS结果的最强因素。二分法的24小时NIHSS得分≤7是第二好的预测因素。
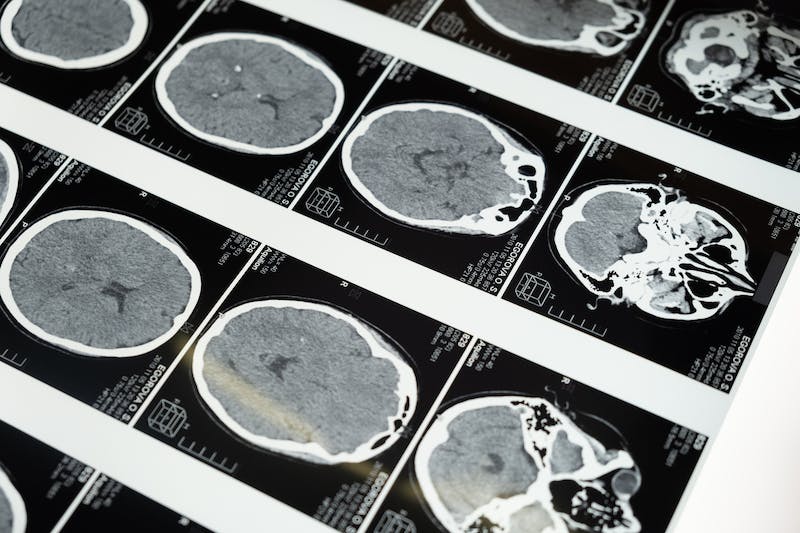
随着围绕急性缺血性卒中血管内治疗(EVT)后的研究进展,提高研究效率的策略变得势在必行。高效的EVT临床试验设计的一个重要组成部分是定义一个早期和最佳的临床替代终点,可以在一定程度上精确区分有效和无效的干预。
此外,对神经系统状态的基线和早期随访(通常是24小时)评估,最经常使用的是美国国立卫生研究院中风量表(NIHSS)评分,是常规且容易进行的。
根据NIHSS测量的早期神经系统状态与以患者为中心的长期功能结果密切相关。因此,急性卒中干预后的NIHSS早期测量是临床试验中一个有吸引力的早期替代临床终点。
然而,这一终点的定义和统计分析在急性卒中文献中存在很大差异。以往的试验认为,NIHSS评分绝对值减少4、8或10分,或24小时NIHSS评分为0-1分,反映早期神经系统恢复。
因此,24小时NIHSS经常被分析为二元结果,往往没有对基线测量进行适当的核算,以使效率提高。
藉此,美国Vanderbilt University Medical Center的Eva A. Mistry等人,利用一个大型的、前瞻性的、现代的、多中心的、真实世界的数据集来确定早期的、基于NIHSS的结果测量,以最好地预测接受EVT治疗的患者的90天功能结果,并利用外部数据集验证这一发现。、
在这项前瞻性观察研究的事后分析中,他们比较了24小时评估的NIHSS、ΔNIHSS(基线减去24小时评估的NIHSS)和百分比变化(NIHSS×100/基线NIHSS)的能力。
使用逻辑回归(调整了年龄、基线NIHSS、葡萄糖、高血压、Alberta Stroke Program早期CT评分、再通时间、再通状态和静脉溶栓)和Spearman ρ,以连续和二分法分析预测90天改良的Rankin量表(mRS)。
在在BEST(Blood Pressure After Endovascular Stroke Therapy)队列的485名患者中,446名(92%)有90天的随访数据被纳入。在多变量模型中对基线进行调整的绝对24小时NIHSS,在所有评估的定义中具有最高的预测能力;
对于用临界点预测mRS评分0-2,这是第二种最有效的方法,24小时NIHSS评分的最佳阈值是≤7(敏感性80.1%,特异性80.4%,P<0.001),其次是NIHSS的百分比变化(敏感性79%,特异性58.5%;P<0.001)。
这个研究的重要意义在于发现了:经基线调整后的24小时NIHSS,是预测血管内治疗患者90天mRS结果的最强因素。二分法的24小时NIHSS得分≤7是第二好的预测因素。
尽管连续的和二分法的NIHSS≥4分可以预测90天的结果,但绝对的24小时评估的NIHSS预测效果更好。
原文出处:
Mistry EA, Yeatts S, de Havenon A, et al. Predicting 90-Day Outcome After Thrombectomy: Baseline-Adjusted 24-Hour NIHSS Is More Powerful Than NIHSS Score Change. Stroke. 2021;52(8):2547-2553. doi:10.1161/STROKEAHA.120.032487
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#24小时#
43
#脑血栓#
55
#NIHSS#
42
#NIH#
47
学习
87
学习
72
nice
74
学习学习
67