Hepatol Int:安罗替尼(Anlotinib)治疗晚期肝细胞癌(HCC)的疗效和安全性:来自ALTER‑0802研究结果
2021-05-22 yd2015 MedSci原创
安罗替尼(Anlotinib)一线或二线治疗晚期肝细胞癌(HCC)有效,并且毒性可控可耐受。并且,血浆CXCL1有可能是安罗替尼的疗效预测因子。
即使现在越来越多抗血管的药物或联合方案应用于晚期肝细胞癌(HCC),但是患者的预后仍然很差。而且,这些药物的最终的耐药很可能跟纤维生长因子受体(FGFR)通路有关。同时也缺乏有效的疗效预测因子。我们知道,安罗替尼(Anlotinib)是一种多靶点的TKI,可以靶向血管内皮生长因子受体(VEGFR) 1–3, 血小板衍生生长因子受体(PDGFR) α/β, FGFR 1–4和 c-kit。体内试验证实安罗替尼能够明显抑制肝细胞癌细胞的生长和促进凋亡。动物试验也发现安罗替尼能够减少HCC的进展。因此,安罗替尼有可能对HCC起作用。基于此目的,来自我国医学科学院肿瘤医院的团队开展了一项II期临床试验((NCT02809534),主要评估安罗替尼一线或二线治疗晚期HCC的疗效和安全性。近期,研究成果发表在Hepatology International杂志上。

该研究为开放标签的II期临床试验。纳入标准:18–75岁局部进展或转移性HCC, 不适合局部治疗,包括TACE、消融、放疗和手术。Child–Pugh < 8,ECOG PS 0- 1,至少一处可测量病灶,和重要功能良好。排除标准:肝胆管细胞癌,或混合癌,HBV DNA > 2000 IU/ml,既往或准备肝移植,出血倾向和脑转移瘤。
纳入的患者分为2队列,其中队列1为既往没有接受TKI治疗的患者;队列2为一线接受TKI治疗的患者。主要研究终点为12周无进展期(PFS)率,次要终点为进展时间(TTP), 客观缓解率(ORR), 总生存期(OS), 24周PFS率和安全性。

研究概况
研究纳入2016年10月至2019年4月期间共50例患者,其中队列1有26例患者,队列2有24例患者。队列1的患者中,12周的PFS率为80.8%(95% CI, 59.8%–91.5%), 24周的PFS率为54.2%(95% CI 32.4–71.7%);TTP为5.9个月 (95% CI 4.8–6.9);中位OS 为12.8个月(95% CI 7.9–20.1)。1例患者 (3.9%) 达到部分缓解(PR),21例患者 (80.8%) 达到稳定(SD)。
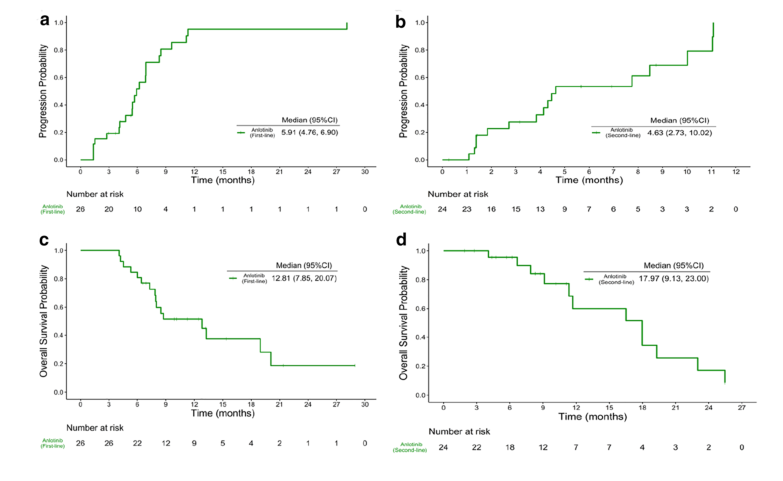
两队列的PFS和OS
队列2的患者中,12周的PFS率为72.5% (95% CI 48.7%–86.6%), 24周的PFS率为46.6% (95% CI 24.4–66.2%);TTP为4.6个月 (95% CI 2.7–10.0),中位OS为18个月(95%CI 9.1–23.0)。2例(8.3%)患者达到PR,16例(66.7%)患者达到SD。

两队列的生存疗效汇总
两队列研究中,患者的基线血浆中CXCL1的水平低于7.6 ng/μl时其TTP均较长。 队列1中,CXCL1大于和小于7.6 ng/μl的患者中位TTP分别为5.9个月(95% CI 1.4–6.9) 和9.1个月(95% CI 6.9–11.2),达到统计学差异(p = 0.0071)。而在队列2中,CXCL1大于和小于7.6 ng/μl的患者中位TTP分别为2.8个月 (95% CI 1.1–7.8) 和10.0个月(95% CI 2.7–11.7), 同样达到条件下差异(p = 0.0029)。
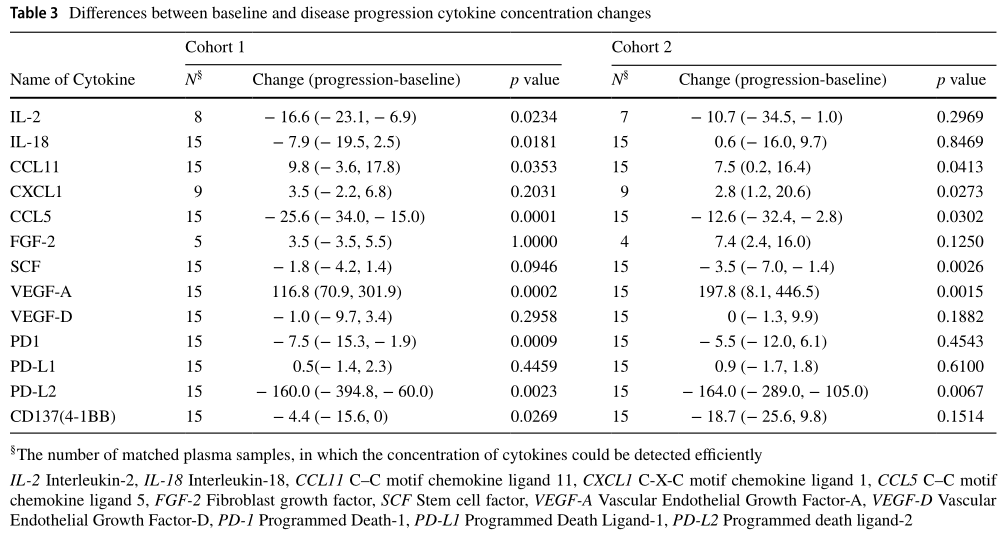
安罗替尼疗效预测因子
常见的不良事件为高血压和甲减(both 62%, 31/50), 接着为疲劳(56%), 手足综合征(54%), 胆红素升高 (52%)和腹泻(52%)。最常见的3-5级不良事件为高血压(8%), 腹泻(8%) 和手足综合征(6%)。5例严重的不良反应中其中2例为安罗替尼相关,都是3级的胃肠道出血。经过治疗,1例恢复,1例死亡。
综上,安罗替尼(Anlotinib)一线或二线治疗晚期肝细胞癌(HCC)有效,并且毒性可控可耐受。并且,血浆CXCL1有可能是安罗替尼的疗效预测因子。
原始出处:
Yongkun Sun, Aiping Zhou, Wen Zhang, et al. Anlotinib in the treatment of advanced hepatocellular carcinoma: an open‑label phase II study (ALTER‑0802 study). Hepatol Int. 2021 Apr 7. doi: 10.1007/s12072-021-10171-0. Online ahead of print.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ALT#
0
#研究结果#
43
#疗效和安全性#
33
#细胞癌#
44
#肝细胞#
43
#HCC#
45
#晚期肝细胞癌#
38
#EPA#
33
谢谢梅斯提供这么好的信息,学到很多
0
没积分
62