Front Oncol:转移性结直肠癌(mCRC)患者使用标准的一线治疗时,KRAS G12C突变与其他亚型对于治疗的应答以及预后的比较
2021-10-03 yd2015 MedSci原创
在一线标准治疗mCRC患者中,与其他突变亚型相比,KRAS G12C突变患者的应答率更低,而中位PFS和OS没有统计学差异。
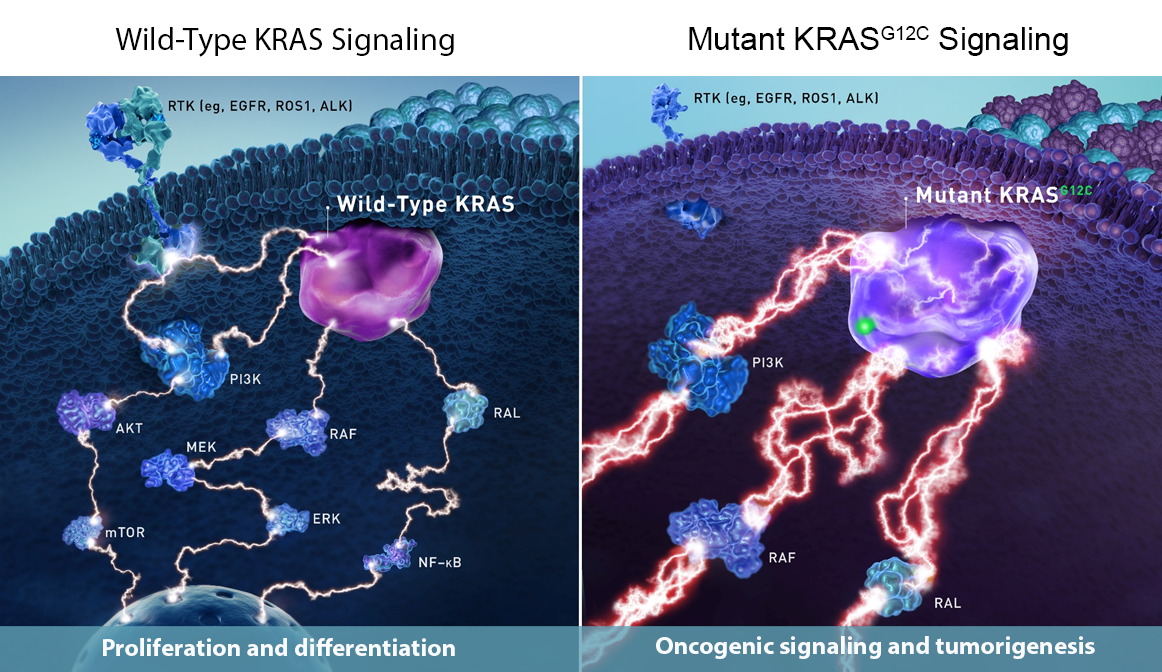
伴有KRAS突变的转移性结直肠癌(mCRC)通常对抗EGFR治疗产生原发性耐药。KRAS突变包括多种亚型,比如G12C,G12D, G12A以及G12V等。其中G12C在KRAS突变的mCRC中约有9–10%。因此,是否所以的亚型对于治疗都是一样的应答或耐药,目前还不是很明确。在肺癌中,G12C亚型的患者通常跟较差的预后相关,而在mCRC还不清楚。近期,来自西班牙的团队开展了回顾性研究,评估在mCRC患者使用标准的一线治疗时,KRAS G12C突变与其他亚型对于治疗的应答以及预后的比较。相关结果发表在Frontiers in Oncology杂志上。

接受FOLFIRI/FOLFOX/ XELOX + Bevacizumab方案一线治疗的KRAS突变mCRC患者纳入研究。排除含有NRAS突变或同时表达BRAF突变的患者。
120例患者最终纳入研究分析,其中KRAS G12C突变15例(12%),KRAS G12D突变48/120例(40%),KRAS G12V突变32/120例(27%),其余25/120例患者KRAS突变与G12C、G12D、G12V不同。

KRAS突变分布
在整个队列中,59/120(49%)的患者达到部分缓解(PR), 42/120(35%)的患者病情稳定(SD), 19/120(16%)的患者病情进展(PD)。中位PFS为9.54个月(95% CI: 8.52 10.78),中位OS为24.85个月(95% CI: 21.18 73.04)。
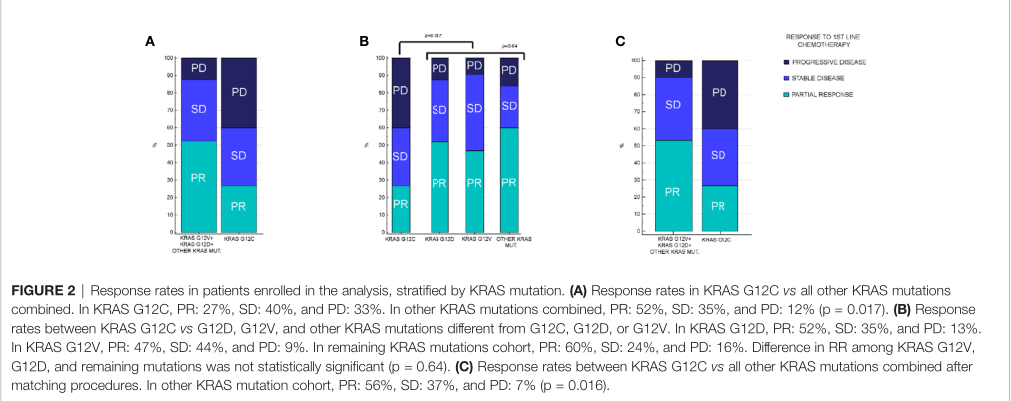
疗效应答
在KRAS G12C突变患者中,4/15(27%)为PR, 6/15(40%)为SD,其余5/15(33%)为PD。在其他KRAS突变的患者中,55/105(52%)为PR, 37/105(35%)有SD,其余13/105(12%)为PD。KRAS G12C突变患者与其他KRAS变异患者的应答率(RR)差异有统计学意义(p=0.017)。
在KRAS G12D突变的患者中,PR为25/48例 (52%),SD为17/48例 (35%),PD为6/48例(13%),而在KRAS G12V突变患者中,PR为15/32例 (47%),SD为14/32例(44%),PD为3/32例(9%)。最后,在其他与G12C、G12D或G12V突变不同的KRAS患者中,15/25例(60%)为PR, 6/25例(24%)为SD,其余4/25例(16%)为PD。比较三种不同突变患者RR无统计学差异(p=0.64)。
G12C突变组患者的mPFS为8.62个月,而其他KRAS突变组患者的mPFS为9.83个月(HR=1.1, 95%CI: 0.55 2.20, p=0.76)。G12C突变组患者的中位OS为37.31个月,而其他KRAS突变患者的中位OS为24.72个月(HR=0.82, 95%CI: 0.44-1.52, p=0.56)。G12C vs G12D vs G12V vs 其他突变对比在中位PFS (p=0.83)和中位OS (p=0.44)均没有差异。

PFS

OS
经过倾向性评分匹配后,KRAS G12C突变患者与其他KRAS变异患者的应答率(RR)差异仍有统计学意义(p=0.016),而中位PFS (HR: 1.24, 95%CI:0.58–2.67, p=0.55)以及中位OS (HR:0.98, 95%0.47-2.08,p=0.97)仍然没有统计学差异。
KRAS G12C与其他KRAS突变在转移转移部位方面也没有统计学差异(肝转移p=1,肺转移p=0.56,腹膜转移p=0.51)、性别(p=0.06)和ECOG PS (p=0.21)。另一方面,与其他KRAS突变相比较,同时性转移(p=0.039),年龄>75岁(p=0.043)和黏液组织学(p=0.008)在G12C突变肿瘤中更常见。
综上,在一线标准治疗mCRC患者中,与其他突变亚型相比,KRAS G12C突变患者的应答率更低,而中位PFS和OS没有统计学差异。
原始出处:
Giampieri R, Lupi A, Ziranu P, Bittoni A, Pretta A, Pecci F, Persano M, Giglio E, Copparoni C, Crocetti S, Mandolesi A, Faa G, Coni P, Scartozzi M and Berardi R (2021) Retrospective Comparative Analysis of KRAS G12C vs. Other KRAS Mutations in mCRC Patients Treated With First-Line Chemotherapy Doublet + Bevacizumab. Front. Oncol. 11:736104. doi: 10.3389/fonc.2021.736104
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
27
#mCRC#
56
#CRC#
39
#KRAS#
64
#转移性#
37
#结直肠#
36