Lancet:挑战指南!血小板功能监测并没有改善冠状动脉内支架植入术治疗ACS老年患者的临床结局 (ANTARCTIC)
2016-08-29 MedSci MedSci原创
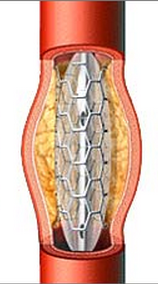
老年患者是缺血性和出血事件的高危患者。血小板功能监测为个体化抗血小板治疗提供了可能以提高治疗的风险效益比。本研究旨在评估急性冠脉综合症安放支架的老年患者中血小板功能检测及治疗调整的效果。 在此多中心开放标签随机对照试验在法国的35个中心进行。纳入75岁以上行冠状动脉支架置入术治疗急性冠状动脉综合征的患者。随机分配(1:1)分别接受口服普拉格雷,每日5毫克,或在反应不足情况下调整药物(监测组)
老年患者是缺血性和出血事件的高危患者。血小板功能监测为个体化抗血小板治疗提供了可能以提高治疗的风险效益比。本研究旨在评估急性冠脉综合症安放支架的老年患者中血小板功能检测及治疗调整的效果。
此多中心开放标签随机对照试验在法国的35个中心进行。纳入75岁以上行冠状动脉支架置入术治疗急性冠状动脉综合征的患者。随机分配(1:1)分别接受口服普拉格雷,每日5毫克,或在反应不足情况下调整药物(监测组);和口服普拉格雷,每天5毫克,但是并不监测和调整治疗(常规组)。血小板功能试验在监测组患者随机后14天和调整治疗后14天完成。
主要研究终点包括随访12个月内心血管死亡、心肌梗死、脑卒中、支架内血栓形成,紧急血运重建,以及出血学术研究联合会定义的出血并发症(2,3,或5型)。研究中做了意向治疗分析。
结果2012年3月27日至2015年5月19日期间随机分配877名患者至监测组(n = 442)或常规组(n = 435)。监测组120名(28%)患者达到了主要终点,常规组123名(28%)患者(危险比(HR),1.003,95% CI 0 . 78 –1.29;P = 0.98)。组间出血事件的发生率无显著性差异。
总而言之,治疗调整的血小板功能监测并没有改善冠状动脉内支架置入治疗急性冠脉综合征的老年患者的临床结局。在许多中心和国际指南中仍推荐高危患者使用血小板功能测试。而该研究结果并不支持这种做法或这些建议。
原始出处:
Guillaume Cayla, Thomas Cuisset, et al., Platelet function monitoring to adjust antiplatelet therapy in elderly patients stented for an acute coronary syndrome (ANTARCTIC): an open-label, blinded-endpoint, randomised controlled superiority trial. The Lancet, DOI: http://dx.doi.org/10.1016/S0140-6736(16)31323-X.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
22
#临床结局#
35
#TARC#
24
文章很好值得关注
57
学习了,赞一个!
73
己拜读,受益匪浅
63
很好,不错,以后会多学习
60
#支架植入#
39
#ACS#
26
#植入#
26