CCR:新研究在CTC中发现与前列腺癌治疗抵抗有关的标记物
2016-09-29 佚名 生物谷
来自美国杜克癌症研究所的研究人员一直在寻找一种非侵入性方式来检测血液中循环的前列腺癌细胞,在这一过程中他们发现了一些与肿瘤抵抗激素治疗有关的血液标记物。这项研究发表在国际学术期刊Clinical Cancer Research上。该研究报道称他们利用一种新技术在循环的前列腺肿瘤细胞中发现多个关键基因的变化,参与研究的这些病人已经对阿比特龙(一种雄激素拮抗药)和恩扎鲁胺这两种药物的治疗产生抵抗。恩扎
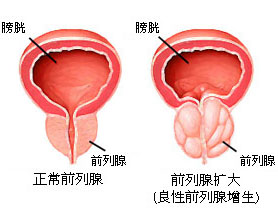
来自美国杜克癌症研究所的研究人员一直在寻找一种非侵入性方式来检测血液中循环的前列腺癌细胞,在这一过程中他们发现了一些与肿瘤抵抗激素治疗有关的血液标记物。这项研究发表在国际学术期刊Clinical Cancer Research上。
该研究报道称他们利用一种新技术在循环的前列腺肿瘤细胞中发现多个关键基因的变化,参与研究的这些病人已经对阿比特龙(一种雄激素拮抗药)和恩扎鲁胺这两种药物的治疗产生抵抗。恩扎鲁胺能够阻断雄激素受体,阿比特龙则可以降低睾丸酮水平。这两种药物都得到批准用于治疗雄激素抵抗性前列腺癌,但是肿瘤仍然会在几年时间内出现药物抵抗。
该研究发现血液中检测到的循环肿瘤细胞可以提供重要的基因信息,有望在未来指导治疗选择,同时提示了新药物开发可以选择的靶点。
研究人员利用一种基于芯片的比较基因组杂交技术对16名前列腺癌病人血液中的循环肿瘤细胞进行了分析,这些病人处于癌症晚期并出现治疗抵抗,该技术能够帮助确定哪些基因出现了多余的拷贝,那些基因区域被删除掉。
研究人员对之前报道过的参与癌症进展的基因和对于癌症有重要作用的其他基因进行了着重分析,他们发现多个信号途径上的基因出现变化,并且这种改变在病人的循环肿瘤细胞中比较常见。
研究人员表示,他们现在正在进行评估,将这种方法与更高分辨率的DNA突变研究以及RNA转录本检测结合在一起对循环肿瘤细胞进行分析,确定它们与病人疾病进展和治疗抵抗的临床相关性。
如果这些基因变化能够在更大规模的研究中得到证实,就可用作生物标记物,作为基于血液的液体活检的一部分,帮助确定哪种治疗方法最有效。这项研究也为药物开发指出了新的靶点。
原始出处
S. Gupta, J. Li, G. Kemeny, R. L. Bitting, J. Beaver, J. Somarelli, K. E. Ware, S. Gregory, A. J. Armstrong.Whole genomic copy number alterations in circulating tumor cells from men with abiraterone or enzalutamide resistant metastatic castration-resistant prostate cancer.CCR.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CTC#
31
#标记物#
28
文章很好,继续关注
46
己学习!
49
谢谢分享,,,
60
学习啦,,,,
49
新研究在CTC中发现与前列腺癌治疗抵抗有关的标记物
53