东方会:当PCI遭遇消化道大出血
2022-09-09 中国医学论坛报今日循环 网络
经皮冠状动脉介入(PCI)术后患者发生消化道大出血无疑是心内科医生临床工作中遇到的比较头痛的问题。
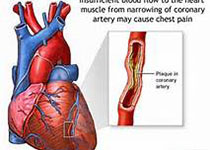
经皮冠状动脉介入(PCI)术后患者发生消化道大出血无疑是心内科医生临床工作中遇到的比较头痛的问题,一边是支架内血栓形成的风险,一边是消化道出血造成的危害,如何权衡利弊?
四大原则请牢记
接受PCI治疗的冠心病患者无论在围手术期还是术后长期,血栓形成风险均明显增高。血小板激活是PCI术后相关血栓形成过程中最关键的因素之一,因此,包括阿司匹林和氯吡格雷在内的充分抗血小板治疗是PCI顺利完成的保证。当PCI术后患者发生消化道大出血时,不要慌张,葛雷教授传授了以下几大治疗原则:联合消化科医生,多学科合作共同商讨,平衡获益与风险以决定是否停用抗血小板药物;大剂量静脉应用质子泵抑制剂(PPI);严格掌握输血指征,必要时给予输血或在内窥镜下进行止血;急性、严重出血的患者需要暂时停用抗血小板药物。
五项细则让处理水平进一步“升级”
输血:患者发生急性出血时应当首先补充晶体液,对血流动力学稳定,血细胞比容>25%或Hb>80 g/L的患者可暂时不输血。经过积极治疗后症状严重出血仍然不能控制的患者可输注血小板。
PPI:行胃镜检查前患者可以口服负荷量的PPI,然后继以静脉输注,根据消化道出血的量和位置,选择继续静脉输注或口服PPI。
内窥镜检查和治疗:早期(24小时之内)的内窥镜检查和治疗可以降低出血、输血和外科手术的风险。若患者出现进行性心肌缺血或心衰有关的低血氧饱和度,则不能耐受内窥镜检查。
中断抗血小板药物治疗:当患者发生严重出血时,阿司匹林和氯吡格雷可以安全停用直到出血情况稳定,在此期间可以依据内窥镜检查结果评估患者持续出血的风险。但某些患者停用抗血小板药物会增加血栓事件的风险,尤其对于急性冠脉综合征(ACS)、置入裸金属支架1个月内、药物涂层支架6个月以内的患者,建议尽量避免完全停用抗血小板药物。阿司匹林导致的消化道出血在经过PPI和(或)内窥镜下止血后,在严密监测下至少观察24小时,如消化道出血无复发,可重新开始抗血小板治疗,但必需与PPI联合用药。
外科手术:当药物和内窥镜治疗仍然无法控制消化道出血时,应当考虑手术治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#东方会#
37
#消化道大出血#
36
#大出血#
41
#消化道#
28