教学相长的力量——上海第九人民医院Cordis下肢动静脉介入手术培训班
2016-05-28 MedSci MedSci原创
在这场归心的路上,一路前行 2016年5月17日-20日由上海第九人民医院血管外科和美国Cordis培训学院共同举办的动静相宜——上海第九人民医院下肢动静脉治疗学习班圆满结束。本次学习班主要针对下肢髂动脉、长段股浅动脉及静脉血栓后综合征的治疗与研究进行了深入的学习与探讨。 [知识与经验的转递] 本次培训班得到了上海第九人民医院血管外科蒋米尔、陆信武等专家教授的大力支持。通
 在这场归心的路上,一路前行
在这场归心的路上,一路前行
2016年5月17日-20日由上海第九人民医院血管外科和美国Cordis培训学院共同举办的动静相宜——上海第九人民医院下肢动静脉治疗学习班圆满结束。本次学习班主要针对下肢髂动脉、长段股浅动脉及静脉血栓后综合征的治疗与研究进行了深入的学习与探讨。

[知识与经验的转递]
本次培训班得到了上海第九人民医院血管外科蒋米尔、陆信武等专家教授的大力支持。通过20余台介入手术、7场授课,以理论结合实际的方式,深入浅出地为学员们提供了全面且有效的学术展示与指导,针对大家的疑问逐一回答,互相交流,使各位学员对动静脉疾病与治疗知识有了更深的了解,收益颇深。

[科技与技术的撞击]
理论授课的直面交流、手术演示的全程直播,线上线下的多维沟通,专家在边做手术边讲解的过程中,让学员更清晰直观地了解手术操作中的要点与技巧。在线的直播更让千里之外的医生与同道者在同一时间观摩了一场学术盛宴。

理论授课的直面交流、手术演示的全程直播,线上线下的多维沟通,专家在边做手术边讲解的过程中,让学员更清晰直观地了解手术操作中的要点与技巧。在线的直播更让千里之外的医生与同道者在同一时间观摩了一场学术盛宴。

[学员心得剪影]
“这几天令我难忘,收获很大!希望能继续开办类似学习班!”——黄志志 百色人民医院
“感谢九院专家老师这几天的指导,有机会接触到这么多的专家,学到了很多知识,感谢!”——何北 绍武市立医院
“谢谢上海九院,收益颇多!希望将来越来越多的血管外科医生能够参加这种培训,也希望这种培训越办越多,越办越好!”——王旭 济宁市第一人民医院
[教学相长的力量]
上海第九人民医院血管外科和美国Cordis培训学院已共同合办数期不同主题的培训班,通过形式多样的教学方式与互动讨论,让全国各地前来学习与交流的介入医生有了更深的理解与收获。今后我们将会继续不遗余力地推进外周介入手术治疗的交流平台,在搭建学术桥梁的工作上,继续努力;同各位老师在这场归心的路上,一路前行。
用心精至、细心愈研,期待不久后的重逢。
演示病例(一):髂股腘动脉长段CTO 球囊扩张,支架成形术
男,89岁。
左下肢疼痛发凉4年。
查体双下肢等粗等长,无肿胀,腓肠肌松软。左下肢膝关节以下皮肤呈暗红色,皮温低,左股动脉搏动(-),左足背动脉、胫后动脉搏动未扪及,双下肢感觉、运动基减退。

术前CT和造影检查:左髂股腘动脉闭塞,管壁钙化明显,侧支开放较多,膝下动脉可见连续性显影。

治疗步骤:
(图A、B)局麻后Seldinger技术穿刺有侧股动脉,翻山至右侧髂动脉,交换长鞘,v18导丝联合支撑导管顺利进入膝下动脉,Savvylong 3mm×220mm、Savvylong4mm×150mm及P3 4mm×40mm球囊导管依次自股总、股浅、腘动脉及胫腓干动脉行球囊扩张,扩张过程中可见切迹,扩张直至切迹消失
(图A、B)局麻后Seldinger技术穿刺有侧股动脉,翻山至右侧髂动脉,交换长鞘,v18导丝联合支撑导管顺利进入膝下动脉,Savvylong 3mm×220mm、Savvylong4mm×150mm及P3 4mm×40mm球囊导管依次自股总、股浅、腘动脉及胫腓干动脉行球囊扩张,扩张过程中可见切迹,扩张直至切迹消失
(图C)扩张完毕造影可见股总动脉处有造影剂外渗,予以球囊压迫后外渗无改善,取Viabahn 5×50mm支架释放于右股总动脉,再次造影外渗消失。
(图D、E )术毕造影可见髂、股、腘及胫后动脉显影良好,造影剂流速通畅,直达足部。
演示病例(二):股腘动脉长段CTO 球囊扩张,支架成形术(P3段逆穿)
男,60岁。
双下肢间跛发麻发凉半月余。
查体双下肢等粗等长,无肿胀,腓肠肌松软。双侧股动脉搏动减弱,双下肢膝关节以下皮肤皮温低,足背动脉、胫后动脉搏动未扪及,双下肢感觉、运动基减退。

术前CT和造影检查:双股浅动脉中上段闭塞,管壁钙化明显,侧支开放较多,腘动脉中远段及膝下动脉可见连续性显影。

治疗步骤:
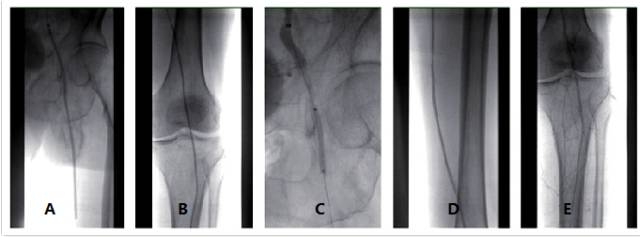
(图A、B)局麻后Seldinger技术穿刺右侧股动脉,翻山至左侧股深动脉,交换长鞘,泥鳅导丝、v18导丝联合支撑导管经内膜下进入股浅动脉闭塞段,经反复尝试无法破膜进入远端真腔。路径下定位左腘动脉P3段,逆行穿刺后置入V18导丝配合支撑导管进入左侧股浅动脉下段,V18导丝顺利进入近端导管,引出体外建立轨迹。取Savvylong 3mm×150mm、4mm×220mm及P3 6mm×100mm自髂动脉、股浅、腘动脉行球囊扩张,扩张过程中可见切迹,扩张直至切迹消失。
(图C、D、E)扩张后造影见左髂动脉斑块回缩明显,取Smart 7×80mm支架定位于左髂总动脉、髂外动脉狭窄闭塞段,在透视下准确释放,支架植入后再次造影提示左髂总、股浅、腘动脉依次显影,造影剂无外渗,血流直达足部。
演示病例(三):PTS球囊扩张,支架成形术
女,46岁。
反复左下肢肿胀2年余。
查体双下肢等长皮温正常。左下肢较对侧肿胀,站立时明显,左小腿少量色素沉着,腓肠肌松软,足背动脉、胫后动脉搏动可扪及。双下肢感觉、运动正常。
(图A、B)局麻后Seldinger技术穿刺右侧股动脉,翻山至左侧股深动脉,交换长鞘,泥鳅导丝、v18导丝联合支撑导管经内膜下进入股浅动脉闭塞段,经反复尝试无法破膜进入远端真腔。路径下定位左腘动脉P3段,逆行穿刺后置入V18导丝配合支撑导管进入左侧股浅动脉下段,V18导丝顺利进入近端导管,引出体外建立轨迹。取Savvylong 3mm×150mm、4mm×220mm及P3 6mm×100mm自髂动脉、股浅、腘动脉行球囊扩张,扩张过程中可见切迹,扩张直至切迹消失。
(图C、D、E)扩张后造影见左髂动脉斑块回缩明显,取Smart 7×80mm支架定位于左髂总动脉、髂外动脉狭窄闭塞段,在透视下准确释放,支架植入后再次造影提示左髂总、股浅、腘动脉依次显影,造影剂无外渗,血流直达足部。
演示病例(三):PTS球囊扩张,支架成形术
女,46岁。
反复左下肢肿胀2年余。
查体双下肢等长皮温正常。左下肢较对侧肿胀,站立时明显,左小腿少量色素沉着,腓肠肌松软,足背动脉、胫后动脉搏动可扪及。双下肢感觉、运动正常。
术中造影(图A、B、C):患者取俯卧位,路径引导下局麻后穿刺左腘静脉,插入7F鞘,鞘内造影提示左股浅静脉中上段、股总静脉、髂静脉管壁僵硬,管腔变细,髋关节及盆腔可讲较多侧枝循环形成。

治疗步骤:
(图D)在导丝导管引导下反复比较顺利通过左髂股静脉狭窄段至下腔静脉,导管内造影证实导管位于下腔静脉内。
(图D)在导丝导管引导下反复比较顺利通过左髂股静脉狭窄段至下腔静脉,导管内造影证实导管位于下腔静脉内。
(图E、F、G、H)分别取P3 6mm×100mm、10mm×80mm、12mm×40mm球囊依次扩张左侧股静脉中上段、髂外、髂总静脉,扩张过程中可见明显腰形切迹,扩张直至切迹消失。鞘内造影可见左侧髂股静脉原病变段可见细线样显影,取Wallstent 12×90mm及Smart 12mm×80mm(2个)支架依次定位左股总静脉至左髂总静脉及下腔静脉原狭窄闭塞段,在透视下准确释放,支架释放后再次造影提示左股静脉、髂静脉及下腔静脉可见连续性显影,支架无移位,造影剂无外渗,盆腔侧支未见明显显影。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#静脉#
33
#人民医院#
48
#Dis#
29
#介入手术#
31
可以去啊
113
值得学习
91