Brit J Cancer:类血管生成素蛋白3能够阻断FAK的细胞核输入并有助于索拉非尼响应
2018-08-01 AlexYang MedSci原创
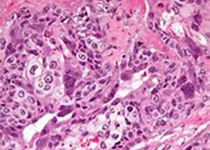
索拉非尼不良的药物反应是一个重要的挑战。不良药物反应减少了肾细胞癌(RCC)患者的临床益处。因此,阐释恢复索拉非尼治疗响应的潜在机制具有中重要的意义。最近,有研究人员利用蛋白免疫印迹和免疫组化技术在2个RCC患者群体中测量了类血管生成素蛋白3(ANGPTL3)含量水平。在RCC细胞中,研究人员利用功能丧失和功能获得试验用来调查ANGPTL3在索拉非尼治疗中的生物学作用,还利用人类蛋白组芯片和免疫沉
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#FAK#
42
#血管生成素#
40
#阻断#
36
#细胞核#
0
了解一下,谢谢分享!
68