PLoS ONE:阻断FGFR抑制肿瘤转移
2012-07-06 Beyond 生物谷
成纤维细胞生长因子受体(FGFR)对肿瘤的生长和癌症病人的生存起着至关重要的作用。相比于其他受体酪氨酸激酶,科学家也一直将成纤维细胞生长因子(成纤维细胞生长因子)作为一种治疗癌症的靶标来开展研究。 近日,研究发现FGFR信号抑制后对原位乳腺66c14癌模型肿瘤生长、转移和淋巴血管形成的影响。体外研究表明FGFR抑制后,66c14细胞增殖比对照组慢。小鼠植入FGFR表达抑制的肿瘤细胞后,66c14
成纤维细胞生长因子受体(FGFR)对肿瘤的生长和癌症病人的生存起着至关重要的作用。相比于其他受体酪氨酸激酶,科学家也一直将成纤维细胞生长因子(成纤维细胞生长因子)作为一种治疗癌症的靶标来开展研究。
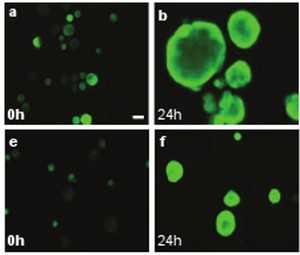
近日,研究发现FGFR信号抑制后对原位乳腺66c14癌模型肿瘤生长、转移和淋巴血管形成的影响。体外研究表明FGFR抑制后,66c14细胞增殖比对照组慢。小鼠植入FGFR表达抑制的肿瘤细胞后,66c14肿瘤的生长和肺转移灶减少,同时有更好的整体生存率。
FGFR表达缺失的肿瘤细胞VEGFR-3(血管内皮生长因子受体3)以及VEGF-C(血管内皮生长因子c)mRNA的表达也减少。这些数据证实成纤维细胞生长因子和血管内皮生长因子对于血管形成是必须的,针对FGFR信号可能是一个非常有前景的抑制肿瘤淋巴管转移和扩散的方法。

doi:10.1371/journal.pone.0039540
PMC:
PMID:
Blocking Fibroblast Growth Factor Receptor Signaling Inhibits Tumor Growth, Lymphangiogenesis, and Metastasis
Frédéric Larrieu-Lahargue, Alana L. Welm, Marion Bouchecareilh, Kari Alitalo, Dean Y. Li, Andreas Bikfalvi*, Patrick Auguste
Fibroblast Growth Factor receptor (FGFR) activity plays crucial roles in tumor growth and patient survival. However, FGF (Fibroblast Growth Factor) signaling as a target for cancer therapy has been under-investigated compared to other receptor tyrosine kinases. Here, we studied the effect of FGFR signaling inhibition on tumor growth, metastasis and lymphangiogenesis by expressing a dominant negative FGFR (FGFR-2DN) in an orthotopic mouse mammary 66c14 carcinoma model. We show that FGFR-2DN-expressing 66c14 cells proliferate in vitro slower than controls. 66c14 tumor outgrowth and lung metastatic foci are reduced in mice implanted with FGFR-2DN-expressing cells, which also exhibited better overall survival. We found 66c14 cells in the lumen of tumor lymphatic vessels and in lymph nodes. FGFR-2DN-expressing tumors exhibited a decrease in VEGFR-3 (Vascular Endothelial Growth Factor Receptor-3) or podoplanin-positive lymphatic vessels, an increase in isolated intratumoral lymphatic endothelial cells and a reduction in VEGF-C (Vascular Endothelial Growth Factor-C) mRNA expression. FGFs may act in an autocrine manner as the inhibition of FGFR signaling in tumor cells suppresses VEGF-C expression in a COX-2 (cyclooxygenase-2) or HIF1-α (hypoxia-inducible factor-1 α) independent manner. FGFs may also act in a paracrine manner on tumor lymphatics by inducing expression of pro-lymphangiogenic molecules such as VEGFR-3, integrin α9, prox1 and netrin-1. Finally, in vitro lymphangiogenesis is impeded in the presence of FGFR-2DN 66c14 cells. These data confirm that both FGF and VEGF signaling are necessary for the maintenance of vascular morphogenesis and provide evidence that targeting FGFR signaling may be an interesting approach to inhibit tumor lymphangiogenesis and metastatic spread.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#阻断#
29
#抑制肿瘤#
26
#Plos one#
29
#肿瘤转移#
32
#FGFR#
25
#GFR#
30