汤敬东:射频消融应对血栓性闭塞性脉管炎第二课
2016-02-16 MedSci MedSci原创
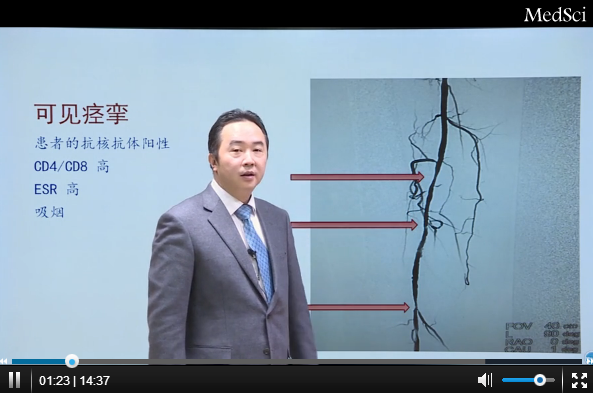
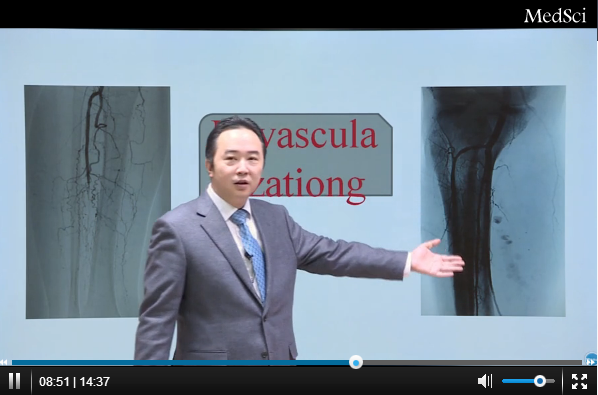
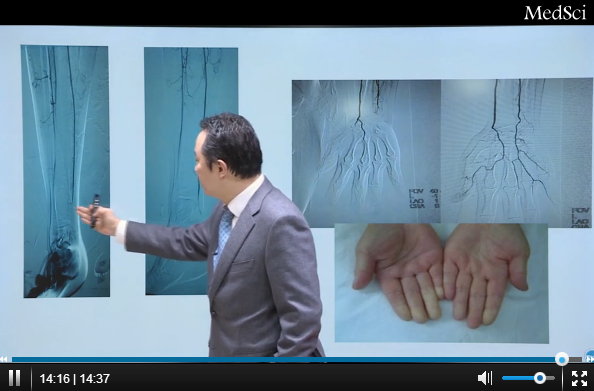
血管闭塞性脉管炎简称脉管炎,是一种进行缓慢的、主要累及四肢中小动脉和静脉的血管病变。中医称“脱疽”。血管闭塞性脉管炎发展历史及病理原理如何?如何应用射频消融术治疗血管闭塞性脉管炎呢?MedSci特别邀请上海交通大学附属第一人民医院血管外科主任医师汤敬东博士为大家讲解,结合临床病例。点击观看汤敬东博士简介:汤敬东,副教授,血管外科博士,博士后。1996.06于第二军医大学获得临床医学学士学位;199
血管闭塞性脉管炎简称脉管炎,是一种进行缓慢的、主要累及四肢中小动脉和静脉的血管病变。中医称“脱疽”。血管闭塞性脉管炎发展历史及病理原理如何?如何应用射频消融术治疗血管闭塞性脉管炎呢?MedSci特别邀请上海交通大学附属第一人民医院血管外科主任医师汤敬东博士为大家讲解,结合临床病例。点击观看
汤敬东博士简介:
汤敬东,副教授,血管外科博士,博士后。1996.06于第二军医大学获得临床医学学士学位;1996.07分配到解放军总医院普外科工作;2003.06于第二军医大学获得外科学(血管外科)硕士学位,同年被聘为普外科主治医师;2007.06于第二军医大学获得外科学(血管外科)博士学位,2007.07-2009.10于复旦大学中山医院血管外科博士后流动站工作,2009.10获复旦大学副教授资格。现工作于上海交通大学附属第一人民医院血管外科。主要学术理念为血流动力学。2000年-2010年主攻方向为主动脉疾病,特别是急性主动脉夹层的诊疗。2010年后主要研究方向为外周血管疾病,特别对血栓闭塞性脉管炎提出了新的理论和治疗探索。共负责国家自然基金1项、省部级课题2项、局级课题1项;主编专着1本、参编专着2本;发表SCI文章5篇,中文核心期刊12篇。
在此非常感谢汤敬东老师将自己经验分享给MedSci的各位朋友,更多课程请登录MedSci学院。(点击进入)
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#血栓性#
20
#射频消融#
39
#消融#
35
好赞收藏
96