Lancet Oncol:局限期小细胞肺癌的放疗标准
2017-06-20 zhangfan MedSci原创
研究发现,对于局限期小细胞肺癌患者,每天两次和每天一次的化疗方法对患者的生存期差异不显著且毒副作用相近。每日一次放疗方法未体现出优越性,甚至没有表现出与每日两次放疗的等效性,这意味着每日两次放疗仍应被视为局限期小细胞肺癌的治疗标准
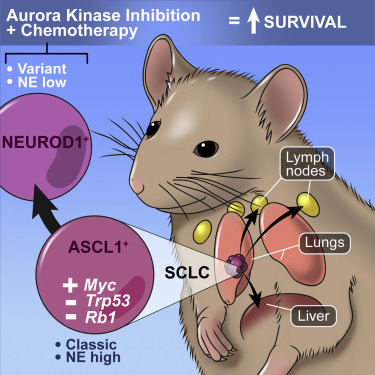
同步放化疗是局限期小细胞肺癌的标准治疗,但最佳的放疗计划和剂量仍然存在争议。近日研究人员开展临床研究旨在建立局限期小细胞肺癌的标准放疗方案。在名为CONVERT的III期研究中,成年的,细胞学或组织学证实的,有足够肺功能的局限期小细胞肺癌0-2期患者参与。患者随机接受总计45Gy,30天每天2次每次1.5Gy的治疗或总计66Gy,3 3天每天1次,每次2Gy的治疗,从治疗的第22天开始进行依托泊苷-顺铂化疗,每3周一次持续4-6轮。主要终点是总生存率。若每日一次组与每日两次组相比,2年的总生存率提高12%,被认为具有临床意义,则显示每日一次方案的优越性。研究招募547名患者,其中每日2次组274人,每日一次组273人。平均随访45个月发现,每日2次组平均生存期为30个月 (95% CI 24-34),每日一次组为25个月(21-31),一次组死亡风险为1.18(95%,CI 0.95-1.45)。2次组患者2年生存率为56% vs 1次组51%(绝对差异5.3%,95%,CI-3.2%-13.7%)。常见的3-4级不良事件发生率:嗜中性白血球减少症(2次vs1次,同下,74% vs 6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
31
#Oncol#
36
挺好的,值得再次学习
60
学习了,谢谢分享
58
制定原则,规范治疗!学习了!
66
不能过度医疗诊治
43
学习了。。。。
58