Cell:重大发现!首次揭示蛋白ANG双管齐下促进造血系统重建
2016-08-14 佚名 生物谷
在一项新的研究中,来自美国塔夫茨大学和塔夫茨医学中心等机构的研究人员发现蛋白血管生长素(angiogenin, ANG)激动人心的新功能:它在调节血细胞形成中发挥着举足轻重的作用,在骨髓移植和促进辐射诱导的骨髓衰竭病人康复中发挥着重要作用。鉴于当前的骨髓移植存在很大的局限性,这些发现可能导致人们开发出重要的治疗性干预来协助改善这些疗法的有效性。相关研究结果发表在2016年8月11日那期Cell期刊
在一项新的研究中,来自美国塔夫茨大学和塔夫茨医学中心等机构的研究人员发现蛋白血管生长素(angiogenin, ANG)激动人心的新功能:它在调节血细胞形成中发挥着举足轻重的作用,在骨髓移植和促进辐射诱导的骨髓衰竭病人康复中发挥着重要作用。鉴于当前的骨髓移植存在很大的局限性,这些发现可能导致人们开发出重要的治疗性干预来协助改善这些疗法的有效性。相关研究结果发表在2016年8月11日那期Cell期刊上,论文标题为“Angiogenin Promotes Hematopoietic Regeneration by Dichotomously Regulating Quiescence of Stem and Progenitor Cells”。
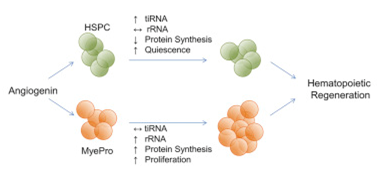
在这篇论文中,研究人员首次证实ANG降低造血干/祖细胞(hematopoietic stem/progenitor cell, HSPC)增殖,同时促进骨髓祖细胞(myeloid progenitor cell)---产生成熟的骨髓细胞---增殖。他们进一步报道这些双管齐下的过程是通过一种新的分子调节机制实现的,这是破天荒第一次取得这样的发现。
这些发现对人HSPC移植和辐射暴露产生重要影响。接受HSPC移植的癌症患者面临两种障碍:短期挑战就是在移植后马上要能产生足够多的白细胞来抵抗可能发生的感染;长期挑战就是保持HSPC功能从而维持体内免疫力。接触大剂量辐射的人面临的挑战就是这些辐射诱导的骨髓衰竭。
论文通信作者、塔夫茨医学中心分子肿瘤学研究所研究员Guo-fu Hu博士说,“我们之前已知道ANG参与促进细胞生长,因此发现ANG促进骨髓祖细胞增殖并不令人意外。但是,令人吃惊的发现是ANG也抑制HSPC生长,而且它是通过细胞类型特异性的RNA加工事件实现这些不同的生长促进或抑制的功能。我们的发现提示着巨大的治疗潜力。”
在一系列实验中,通过与来自美国麻省总医院的科学家合作,研究人员分离出ANG,并描述了它的不同调节功能。他们证实了ANG如何促进骨髓祖细胞增殖。他们证实ANG如何通过诱导一种静息(也被称作细胞休眠)状态来维持HSPC,这也是首次发现ANG具有抑制活性。随着时间的推移,这种静息状态能够维持HSPC,这样它们在未来就可用于维持体内免疫力。
在另一项新的发现中,研究人员证实ANG通过诱导不同的细胞类型发生不同的RNA加工来实现这两种功能的。在HSPC中,ANG诱导一种特定类型的被称作tRNA来源应激诱导性小RNA(tRNA-derived stress-induced small RNA, tiRNA)的RNA产生,其中tiRNA抑制全局蛋白合成,从而促进HSPC进入静息状态;在骨髓祖细胞中,ANG诱导一种特定类型的被称作核糖体RNA(rRNA)的RNA产生,其中rNRA增强蛋白表达,从而促进骨髓祖细胞增加。
论文第一作者Kevin A. Goncalves说,“适当的血细胞产生依赖于功能性的HSPC,然而在移植预处理期间或骨髓损伤之后,HSPC受到破坏。我们的研究证实ANG调节着这两种临床重要的细胞类型的至关重要的功能。”
在进一步的研究中,研究人员测试了ANG阻止和缓解辐射诱导的骨髓衰竭的能力。在临床前模式动物体内,他们发现在接受重组ANG蛋白治疗后,它们在辐射暴露后的存活期增加了。
原始出处
Kevin A. Goncalves, Lev Silberstein, Shuping Li, Nicolas Severe, Miaofen G. Hu, Hailing Yang, David T. Scadden, Guo-fu Hu.Angiogenin Promotes Hematopoietic Regeneration by Dichotomously Regulating Quiescence of Stem and Progenitor Cells.Cell.2016
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







学习了谢谢
75
#重大发现#
25
#CEL#
26
#Cell#
27
#造血#
24