JCEM:利拉利汀对胰岛β细胞具有保护作用
2013-05-14 JCEM dxy
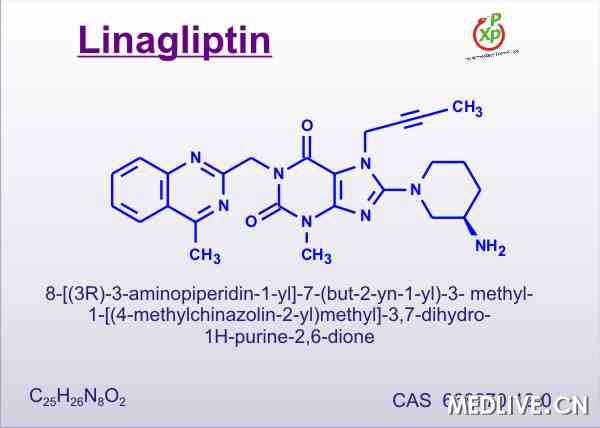
在糖尿病,抑制二肽基肽酶–4(DPP–4)是一种增加GIP和GLP–1,诱导胰岛素分泌的有效治疗策略。了解被批准用于2型糖尿病治疗的新药是否能直接影响β细胞是非常重要的。为了探讨利拉利汀,一种新型的DPP–4抑制剂,对β细胞功能和存活的影响,来自德国不莱梅大学的Kathrin Maedler教授及其团队进行了一项研究,该研究发现新型的DPP–4抑制剂利拉利汀保护人类胰岛不受糖毒性、脂毒性和细胞毒性

在糖尿病,抑制二肽基肽酶–4(DPP–4)是一种增加GIP和GLP–1,诱导胰岛素分泌的有效治疗策略。了解被批准用于2型糖尿病治疗的新药是否能直接影响β细胞是非常重要的。为了探讨利拉利汀,一种新型的DPP–4抑制剂,对β细胞功能和存活的影响,来自德国不莱梅大学的Kathrin Maedler教授及其团队进行了一项研究,该研究发现新型的DPP–4抑制剂利拉利汀保护人类胰岛不受糖毒性、脂毒性和细胞毒性之害,并稳定兴奋人类胰岛分泌GLP-1,提示利拉利汀对β细胞功能和存活具有GLP-1直接介导的保护作用。该研究结果在线发表在2013年4月30日的美国《临床内分泌代谢杂志》(The journal of clinical endocrinology metabolism)上。
该研究中,人类胰岛暴露在伴或不伴有500ng/ml白介素–1受体拮抗剂(IL–1Ra)或30–50nM利拉利汀的糖尿病环境中(11.1–33.3mM葡萄糖,0.5mM棕榈酸,IL–1β2ng/ml+IFN–r 1000U/ml或H2O2 50uM的混合物)。
该研究结果表明,当胰岛暴露于高葡萄糖、棕榈酸酯、细胞因子或H2O2时,利拉利汀修复受损的β细胞功能和存活。IL–1Ra预处理同样有效,但不包括抗H2O2治疗。胰岛裂解物中硝基酪氨酸浓度,一种氧化应激的指标,在糖尿病条件下显著升高,但在利拉利汀或IL–1Ra治疗的胰岛中不升高。在胰岛上清液中,利拉利汀同样减少细胞因子分泌,并稳定GLP–1。
该研究发现,新型的DPP–4抑制剂利拉利汀保护人类胰岛不受糖毒性、脂毒性和细胞毒性之害,并稳定兴奋人类胰岛分泌GLP-1,提示利拉利汀对β细胞功能和存活具有GLP-1直接介导的保护作用。
与利拉利汀相关的拓展阅读:
- IJCP:临床试验表明II型糖尿病药物利拉利汀长期使用有效且安全
- 二甲双胍不能控制的糖尿病患者:利拉利汀2年效果非劣于格列美脲
- [ACCE2012]利拉利汀对非裔2型糖尿病患者安全有效
- 利拉利汀对非裔2型糖尿病患者安全有效 更多信息请点击:有关利拉利汀更多资讯

The DPP-4 inhibitor linagliptin restores β-cell function & survival in human isolated islets through GLP-1 stabilization.
Context
Inhibition of Dipeptidyl peptidase-4 (DPP-4) is a potent strategy to increase GIP and GLP-1 induced insulin secretion in diabetes. It is important to know if new drugs approved for the treatment of type 2 diabetes have direct effects on the β-cell.
Objective
Herein, we investigated the effect of linagliptin, a novel DPP-4 inhibitor, on β-cell function and survival.
Design
Human islets were exposed to a diabetic milieu (11.1-33.3 mM glucose, 0.5 mM palmitic acid, the mixture of 2 ng/ml IL-1β+1,000 U/ml IFN-γ or 50 μM H2O2) with or without 500 ng/ml Interleukin-1Receptor Antagonist (IL-1Ra) or 30-50 nM linagliptin.
Results
Linagliptin restored β-cell function and turnover, which was impaired when islets were exposed to elevated glucose, palmitate, cytokines or H2O2. Pre-treatment with IL-1Ra was similarly effective, except against H2O2 treatment. Nitrotyrosine concentrations in islet lysates, an indicator of oxidative stress, were highly elevated under diabetic conditions, but not in islets treated with linagliptin or IL-1Ra. Linagliptin also reduced cytokine secretion and stabilized GLP-1 in islet supernatants.
Conclusions
We show that the novel DPP-4 inhibitor linagliptin protected from gluco-, lipo- and cytokine-toxicity and stabilized active GLP-1 secreted from human islets. This provides a direct GLP-1 mediated protective effect of linagliptin on β-cell function and survival.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#胰岛#
22
#胰岛β细胞#
25
#JCE#
32
#JCEM#
31
#保护作用#
44
#β细胞#
36