Cancer Cell:改变肿瘤微环境提高抗癌药物作用
2012-04-20 Beyond 生物谷
近日,冷泉港实验室(CSHL)科学家说:显着改善癌症对现有的“经典”的化疗药物常见的反应,改变癌细胞与周围细胞(肿瘤微环境)的相互作用,可以提高抗癌药物的功效。 冷泉港实验室助理教授Mikala Egeblad和她的研究小组在Cancer Cell杂志发表文章,使用“活体显微镜”观察小鼠肿瘤中的癌细胞对已经广泛使用的化疗药物阿霉素做出反应。他们发现这两个调节肿瘤微环境因子(基质金属蛋白酶(MMP
近日,冷泉港实验室(CSHL)科学家说:显着改善癌症对现有的“经典”的化疗药物常见的反应,改变癌细胞与周围细胞(肿瘤微环境)的相互作用,可以提高抗癌药物的功效。
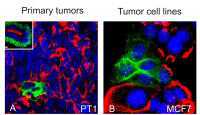
冷泉港实验室助理教授Mikala Egeblad和她的研究小组在Cancer Cell杂志发表文章,使用“活体显微镜”观察小鼠肿瘤中的癌细胞对已经广泛使用的化疗药物阿霉素做出反应。他们发现这两个调节肿瘤微环境因子(基质金属蛋白酶(MMPs)和免疫信号分子趋化因子)的选择性抑制能使得小鼠乳腺肿瘤对药物更加敏感。
众所周知,肿瘤细胞中的基因突变和表观遗传变化有助于肿瘤提高抵抗治疗的能力。但肿瘤组织中除了癌细胞外,还含有许多其他类型细胞。令人惊讶的一点因素,这些非癌变细胞(基质细胞)分泌的因子是如何影响肿瘤耐药性的。这些基质细胞包括白细胞。
Egeblad的研究小组利用实时显微成像观察了癌细胞对肿瘤微环境中的阿霉素做出了怎么样的反应。研究结果揭示了药物如何随着时间推移移出供给肿瘤营养的血管,在肿瘤不同阶段药物杀死癌细胞的方式和速度以及肿瘤细胞之间的相互作用动力学在用药之前、期间和用药后。
Egeblad说:我们可以清楚地看到微环境有助于药物对肿瘤的作用,微环境通过调控血管通透性或渗漏以及炎性细胞的募集等降低药物作用。
Egeblad表示:缺乏编码MMP9基因的基因工程小鼠体内血管通透性好,肿瘤细胞能更好的响应阿霉素。
她指出,现有的MMP酶抑制剂在临床试验中都失败了。但我们的数据表明这些药物或其他影响血管通透性的药物,可以用来辅助化疗。
冷泉港实验室团队采用实时成像收集技术的另一个重要发现是,肿瘤组织中最常见的非癌变细胞--粒细胞,在化疗期间会持续募集到肿瘤部位。髓细胞往往被吸引到细胞死亡部位。研究小组发现这种吸引力是有CCL2激活信号引发的,CCL2是一类趋化因子,能募集免疫细胞。
通过敲除编码趋化因子受体(CCR2)的基因能够减少髓细胞募集到肿瘤部位。重要的是,这一做法也增加了阿霉素和另一种常用的化疗药物顺铂的药效。
冷泉港实验室团队现通过确定肿瘤化疗期间如何募集髓细胞的,正在寻找提高响应化疗的肿瘤治疗方式。

doi:10.1016/j.ccr.2012.02.017
PMC:
PMID:
Imaging Tumor-Stroma Interactions during Chemotherapy Reveals Contributions of the Microenvironment to Resistance
Elizabeth S. Nakasone, Hanne A. Askautrud, Tim Kees, Jae-Hyun Park, Vicki Plaks, Andrew J. Ewald, Miriam Fein, Morten G. Rasch, Ying-Xim Tan, Jing Qiu, Juwon Park, Pranay Sinha, Mina J. Bissell, Eirik Frengen, Zena Werb, Mikala Egeblad
Little is known about the dynamics of cancer cell death in response to therapy in the tumor microenvironment. Intravital microscopy of chemotherapy-treated mouse mammary carcinomas allowed us to follow drug distribution, cell death, and tumor-stroma interactions. We observed associations between vascular leakage and response to doxorubicin, including improved response in matrix metalloproteinase-9 null mice that had increased vascular leakage. Furthermore, we observed CCR2-dependent infiltration of myeloid cells after treatment and that Ccr2 null host mice responded better to treatment with doxorubicin or cisplatin. These data show that the microenvironment contributes critically to drug response via regulation of vascular permeability and innate immune cell infiltration. Thus, live imaging can be used to gain insights into drug responses in situ.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#药物作用#
39
#CEL#
37
#Cell#
24
#cancer cell#
40
#抗癌药物#
0
#抗癌药#
33