JAMA Netw open:血清尿酸水平与肾大血管和微血管功能障碍的关系
2021-10-29 MedSci原创 MedSci原创
SUA浓度与肾脏微血管功能障碍之间的联系部分通过血压介导。
普通人群中动脉粥样硬化性疾病很常见,如冠状动脉疾病(CAD)、外周动脉疾病(PAD)和脑血管疾病,且常并发急性冠状动脉综合征、严重肢体缺血和脑血管意外等。同样,肾病微血管病变也普遍存在,并且是肾衰竭的主要病因。
在欧亚人群中,血清尿酸(SUA)水平与血管功能障碍相关,但对于撒哈拉以南的非洲人群来说,这种相关性知之甚少,他们的SUA水平和血管功能障碍的患病率都很高,因此有研究者选取了2012年至2015年间加纳人的健康数据来进行了相关研究。
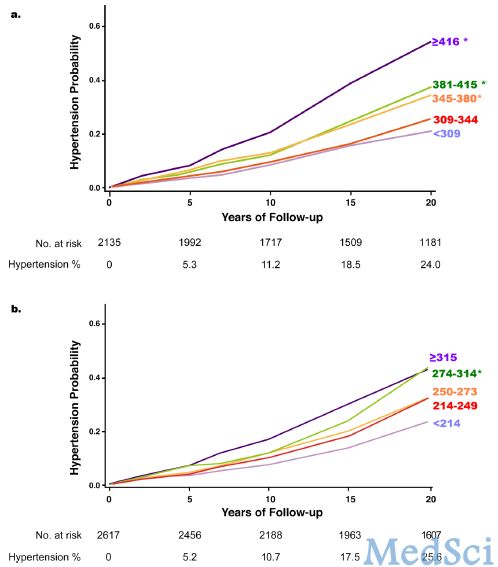
通过Logistic回归分析SUA与微血管(蛋白尿)和大血管(外周动脉疾病和冠状动脉疾病)功能障碍的相关性,并调整年龄、性别、估计肾小球滤过率、居住地点、社会经济状况、酒精、吸烟、糖尿病、高血压、腰臀比和总胆固醇水平。进行中介分析,以评估该相关性是否与血压升高、血红蛋白A1c和高敏C反应蛋白水平有关,或与体重臀围比有关。
共有4919名加纳人(3047名[61.9%]妇女)参与了本研究,年龄在25-75岁之间。校正协变量后,SUA四分位数与蛋白尿之间存在显著正相关,但与冠状动脉疾病或外周动脉疾病之间无显著正相关。在完全调整后,与第一个四分位数的个体相比,第四个SUA四分位数的个体有更高的蛋白尿几率,但没有外周动脉疾病或冠状动脉疾病。完全调整后,收缩压和舒张压显著介导SUA浓度与蛋白尿之间的相关性,占收缩压和舒张压总相关性的19.4%和17.2%;血红蛋白A1c、高敏C反应蛋白和腰臀比并不介导这种关联。

SUA与大血管和肾脏微血管功能障碍的关系
本研究表明,在南非患者人群中,较高的SUA浓度与肾脏微血管功能障碍相关,而与大血管功能障碍无关。SUA浓度与肾脏微血管功能障碍之间的联系部分通过血压介导。SUA水平升高的患者可能受益于肾脏微血管功能障碍的定期筛查,以帮助早期发现和治疗。
参考文献:Hayfron-Benjamin CF, van den Born B, Amoah AGB, et al. Associations of Serum Uric Acid Levels With Macrovascular and Renal Microvascular Dysfunction Among Individuals From Sub-Saharan Africa. JAMA Netw Open. 2021;4(10):e2128985. doi:10.1001/jamanetworkopen.2021.28985
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#大血管#
37
#微血管功能障碍#
27
#PE#
29
#NET#
34
#微血管#
37
#功能障碍#
27
#血清尿酸#
30
#血管功能#
39
不错,学习了
61