【一般资料】
患者男性,38岁,
【主诉】
因左眼鼻侧黑影遮挡2d,2013年8月22日于天津医科大学眼科医院入院。
【既往史】
患者既往双眼高度近视眼,屈光度数为-13.00D,双眼先天性眼球震颤。
【家族史】
患者父母非近亲结婚,家族无其他患白化病者,患者父母及弟弟妹妹、独子均未有类似表现。
【体格检查】
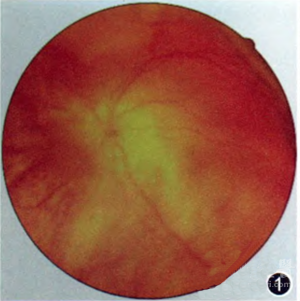
入院时检查发现毛发色淡,余无异常。眉毛和睫毛有少许白色。眼部检查:右眼视力0.1,矫正0.12,眼压14.6mmHg(1mmHg=0.133kPa),眼球钟摆性震颤,前节(-),眼底可见视盘界清色可,视网膜呈豹纹状,后极部RPE无色素,透见粗大的脉络膜血管。左眼视力眼前手动,矫正不提高,眼压9.4mmHg,眼球钟摆性震颤,前节(-),眼底可见4~6点钟方位视网膜波浪形隆起,累及黄斑区,1点钟方位可见一马蹄形裂孔,大小约3/4PD,后极部RPE无色素,透见粗大的脉络膜血管(图1)。
【辅助检查】
B超示左眼视网膜脱离,OCT示左眼黄斑颞侧神经上皮层脱离。
【初步诊断】
左眼孔源性视网膜脱离,双眼白化病眼底改变,双眼先天性眼球震颤,双眼高度近视,双眼高度近视性视网膜病变。
【治疗】
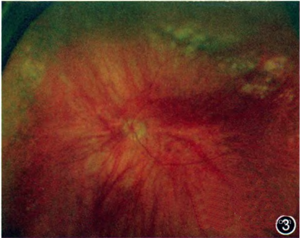
2013年8月23日局部麻醉下行左眼玻璃体切除术+气液交换+视网膜光凝+硅油填充术。术后眼部检查:左眼视力0.1,+5.00D矫正至1.2,眼压12.9mmHg,玻璃体腔硅油填充,眼底可见后极部RPE无色素,透见粗大的脉络膜血管,裂孔闭合,网膜在位(图2)。2014年3月10日局部麻醉下行左眼硅油取出术。术后眼部情况:左眼视力0.02,眼压13.7mmHg,视网膜在位。后患者视力逐渐下降,检查发现晶状体混浊,视网膜在位。2015年3月20日局部麻醉下行左眼白内障超声乳化联合人工晶状体植人术。2016年1月3日患者再次就诊,主因左眼鼻侧黑影遮挡2d入院。眼部检查:左眼视力0.08,眼压13mmHg,前节(-),眼底上方10点至2点视网膜隆起,上方赤道部变性带上可见裂孔(图3)。B超示左眼视网膜脱离。局部麻醉下行左眼玻璃体切除+视网膜光凝+C3F8填充术。术后1周左眼视力眼前手动,眼压10mmHg,玻璃体腔气体填充约占1/2。术后23d再次复诊,患者主诉左眼固定暗影遮挡。眼部检查:左眼视力0.04,眼压13mmHg,眼底可见下方4-8点钟方位视网膜隆起,累及黄斑。B超示左眼玻璃体腔内点状强回声,前部少量杂乱强回声,下方强回声膜状光带后连球壁。局部麻醉下行左眼玻璃体切除+硅油填充术。术后查体:左眼视力0.1,眼压20mmHg,玻璃体腔硅油填充,眼底网膜复位。

版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#白化病##视网膜脱离#
69
#复发性#
58
学习了.谢谢作者分享!
86
#视网膜#
44
学习一下谢谢
86