Asia Pac Allergy:2016年墨尔本风暴性哮喘流行分析:哮喘、鼻炎和其他过敏症
2017-11-10 AlexYang MedSci原创
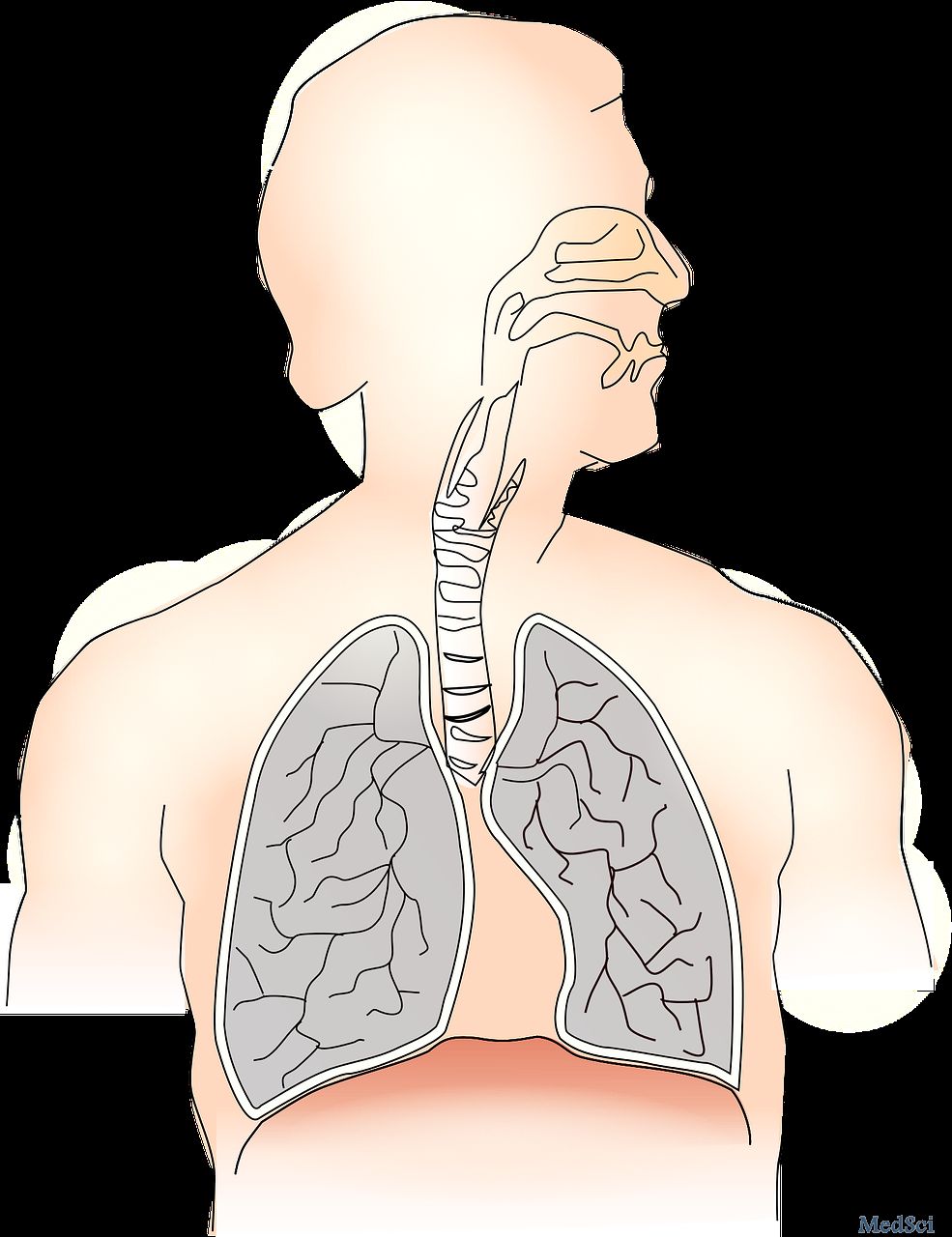
2016年11月21日,墨尔本经历了风暴性哮喘流行。尽管在以前的文献中有所报道,风险因素和自然史仍旧没有完全阐释。最近,有研究人员跟踪调查了在流行期间,在他们的急诊室(EDs)就医的病人,并且对他们以往的哮喘、鼻炎和过敏症进行了评估。研究人员回顾了对在风暴事件48小时内的所有呼吸道表现的ED记录,并且包括了急性哮喘的病人。另外,研究人员还围绕哮喘诊断、未诊断哮喘症状和鼻炎程度设计了标准化的调查问卷
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ASIA#
36
#墨尔本#
30
#ALL#
36
#过敏症#
37
学习了.好文章
79