JACC子刊:中山医院结构团队的两项中国原创器械研究结果公布
2022-06-18 瓣膜中心 瓣膜中心
近日,中山医院葛均波院士、周达新教授、潘文志主任医师领衔的结构团队在国产原创医疗器械上取得重要研究成果,2项国产原创医疗器械的研发与转化项目分别以标题“Feasibility Study
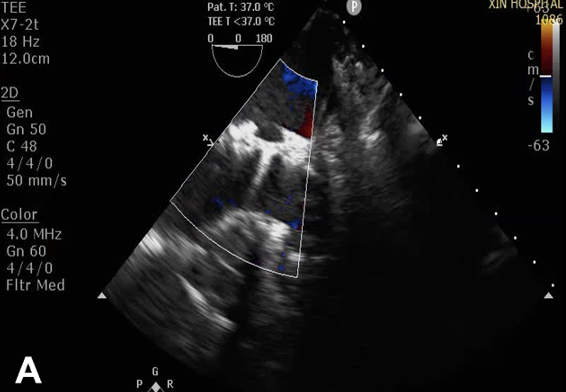
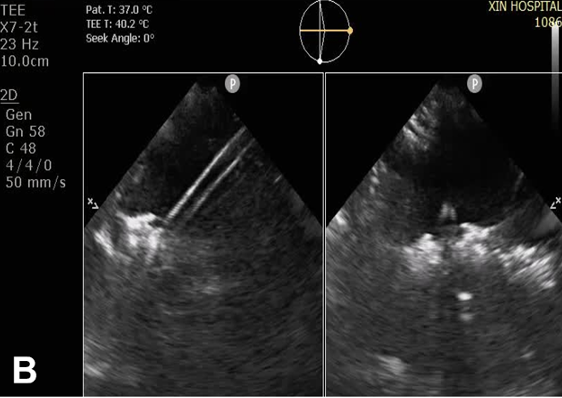
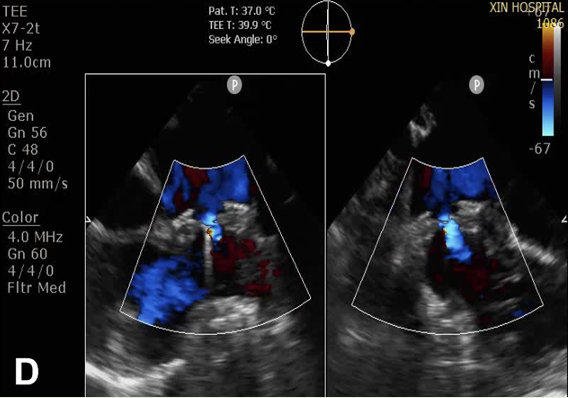
近日,中山医院葛均波院士、周达新教授、潘文志主任医师领衔的结构团队在国产原创医疗器械上取得重要研究成果,2项国产原创医疗器械的研发与转化项目分别以标题“Feasibility Study of a Novel Transcatheter Tricuspid Annuloplasty System in a Porcine Model(一种新型经导管三尖瓣瓣环成形系统的临床前研究)”,“A novel puncturable atrial septal defect occluder: The short-term results of preclinical experiment and first-in-human study(一种新型可穿刺房间隔封堵器的临床前研究以及探索性临床研究)”,被转化医学领域顶尖期刊《JACC:Basic to Translational Science》以原创论著形式接受。 第一项原创器械转化的研究瞄准的是国际最前沿的三尖瓣反流的微创介入治疗,报道了世界首个经导管三尖瓣瓣环成形夹(K-Clip,上海汇禾)的临床前研究结果,证实了其在大动物模型上的可行性。 三尖瓣既往是“被遗忘的瓣膜”,但近年来越来越多的临床证据表明:重度的三尖瓣反流会显著增加患者心衰的风险,导致预后不良。并且三尖瓣反流主要是功能性的,即三尖瓣瓣环扩张导致瓣叶闭合不良。外科三尖瓣(环缩)成形是治疗重度三尖瓣反流的标准治疗方法,但是外科手术的风险很高,特别是既往有过外科手术史的患者,因此绝大部分患者都只能寄希望于微创介入治疗。 国外的三尖瓣经导管瓣环成形器械至今尚未进入国内,且多用缝线打孔方式进行瓣环环缩,而研究报道的K-Clip器械,使用金属夹子巧妙的将外科三尖瓣环缩的经典术式通过微创介入的方法实现,并且其操作相比国外器械更为简单。其有望成为国内首个上市的经导管三尖瓣环缩器械,填补我国在经导管三尖瓣成形技术的空白,带领我国心脏瓣膜介入治疗步入国际领先行列!K-Clip早期的探索性的临床研究已经在中山医院完成,验证其效果良好。目前该器械的多中心临床研究正在国内进行。 第二项原创器械转化项目报道了世界首个可穿刺房间隔封堵器(ReAces,上海捍宇)的大动物可行性研究和10例探索性临床研究的短期结果。房间隔缺损是常见的先天性心脏病,而房间隔缺损封堵的患者多为年轻病人,这些患者随着年龄的增加,心房颤动、二尖瓣反流等疾病的患病率会高于普通人。而这些疾病,目前临床上成熟的治疗方法分别有:射频消融、左心耳封堵、以及二尖瓣夹合等微创介入手术,但这些术式均需要穿刺房间隔进入左心房进行操作。而现有常规封堵器均为镍钛合金丝密集编网制成,因而封堵之后左右心房之间,将被2-4层密集编织的金属网隔绝,届时要再穿刺房间隔将鞘管从右心房送入左心房成为不可能。患者丧失房间隔这一重要介入治疗通道,也就丧失了后续进行微创介入治疗心房颤动、二尖瓣反流等疾病的机会。 针对目前房间隔缺损封堵治疗存在的技术难题,葛均波院士、周达新教授、潘文志主任医师在国际上首先提出可穿刺房间隔封堵器的概念,申请了国内和国际的专利:这种可穿刺房间隔封堵器,可在保证房间隔缺损封堵器安全有效的前提下,为后续实施房间隔穿刺介入手术保留通道,给予患者进行跨房间隔微创介入手术的机会。研究报道了其在大动物模型上的应用,所有的猪在植入该封堵器后房间隔缺损均被完全封堵,其中4头猪在房间隔封堵后顺利地进行了房间隔的再次穿刺。10例房间隔缺损的患者参加了该封堵器的早期探索性临床研究,这些患者房间隔的缺损平均达14.5±4.8mm,所有患者均一次性成功植入该封堵器,术后超声检查所有患者的房间隔缺损均被完全封闭。该器械目前为国际首创新型器械,国内外均无相似设计产品,是我国原创医疗器械解决国际难题的优异典范!目前,可穿刺房间隔封堵器即将开展其上市前的临床研究。 《JACC:Basic to Translational Science》是美国心脏学会杂志,心血管领域顶级刊物《Journal of the American College of Cardiology》的子刊,其影响因子约10分,是转化医学领域影响力最高的杂志之一,专注于国际最新最具影响力的转化医学研究进展。此次中山医院结构团队两项重磅原创器械研究以论著形式被权威杂志收录,体现中山医院结构团队在转化医学领域的硬实力!


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#结果公布#
59
#研究结果#
47
#JACC#
37
#ACC#
49
#中山医院#
53