J GASTROEN HEPATOL:中科院无创筛查获新突破!做个深呼吸就能诊断癌症
2016-12-15 生物探索 生物探索
导读 近期, 中科院合肥物质科学研究院的研究人员自主研发出实时在线检测呼气质谱仪,被检者只需长呼一口气,3分钟内就能检测出是否患有食管癌,其临床试验准确率达85%至90%。这是我国在癌症无创筛查领域的一个新突破。食管癌是一种常见的恶性肿瘤,在全球范围内的发病率和死亡率分别排在恶性肿瘤的第8和第6位,在我国年发病人数预计47万、死亡人数约37万。开发快速、无创性的食道癌筛查方法是当前相当大的需求。近
导读 近期,中科院合肥物质科学研究院的研究人员自主研发出实时在线检测呼气质谱仪,被检者只需长呼一口气,3分钟内就能检测出是否患有食管癌,其临床试验准确率达85%至90%。这是我国在癌症无创筛查领域的一个新突破。
近期,中国科学院合肥物质科学研究院医学物理与技术中心研究部光谱质谱研究室的研究人员在Journal of Gastroenterology and Hepatology(《肠胃病学与肝病期刊》)上展示了一款自主研发的实时在线检测呼气质谱仪。利用该仪器,被检者只需长呼一口气,3分钟内就能检测出是否患有食管癌,其临床试验准确率达85%—90%。该研究推动了食道癌快速无创筛查的前进步伐,是我国在癌症无创筛查领域的一个新突破。
PTR-MS:食道癌无创筛查的新突破口

呼吸采样系统示意图
研究人员利用自主研发的质子转移反应质谱仪(PTR-MS)测量了29名食管癌患者和57名健康人士呼出的气息,并利用Mann-Whitney U检验和逐步判别分析(stepwise discriminant analysis)来确定呼吸质谱数据中的离子,从而从健康人群中区分癌症患者。此外,该研究还进行了受试者工作特征(receiver operator characteristic,ROC)分析。
研究人员发现7种呼吸质谱离子能区分健康人士和食管癌患者,敏感性和特异性分别为86.2%和89.5%。这7种呼吸质谱离子分别是 m/z 136、m/z 34、m/z 63、m/z 27、m/z 95、m/z 107 和 m/z 45。与健康人相比,食管癌患者呼气质谱分析中有5种质谱离子的中位强度(mediant intensities,编者自译)降低,剩余2个质谱离子的中位强度增加。ROC曲线下面积为0.943。
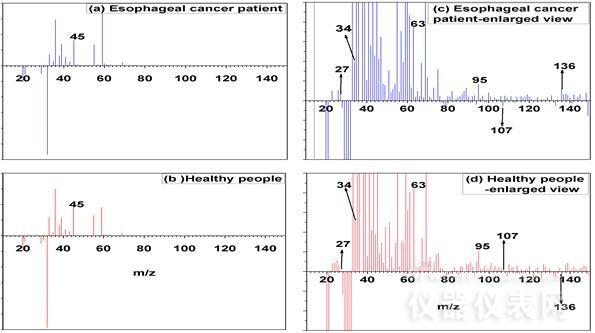
食管癌患者/健康志愿者呼气质谱图
研究人员最后得出以下结论:利用质子转移反应质谱仪(PTR-MS)检测呼出气体中挥发性有机化合物(VOCs)的离子特征,可以区分健康人士和食管癌患者。然而,研究人员认为需要更多的患者呼气试验来证实,但质子转移反应质谱仪(PTR-MS)有望成为一种具有前景的食管癌筛查手段。
新技术避免了以往方法存在的缺陷
目前食管癌临床检查主要依靠X射线钡餐、CT扫描、内窥镜/活检、细胞学检查等方法,这些常规检查需要射线/器械侵入或者有创,不适合体检或高危人群筛查。为了食管癌能早发现,让患者得到早治疗,提高治愈率、降低死亡率,发展食管癌筛查新技术方法尤为重要。
以往的呼气检测研究大多数沿用采样袋呼气取样与色谱质谱离线分析方法,该方法潜在问题是:采样袋易引起呼气成份污染、甚至丢失,色谱质谱分析需要约2个小时。因为质控困难、过程繁琐以及分析速度慢,这种方法难以满足筛查对快速检测的要求。
中科院自主研制的实时在线检测呼气质谱仪,只需7秒钟就能完成对一名受试人员呼气的直接测量,不需要采样袋取样以及浓缩等前处理过程,且仪器连续运行1个月离子信号强度波动仅为1.1%。
癌症无创筛查之呼气检测法
2013年4月,瑞士苏黎世联邦理工学院在PLoS ONE上表明,每个人在呼吸时呼出的化合物和人类的指纹一样独一无二,医生甚至可以根据这些化合物来诊断疾病(如癌症)。呼气检测因为安全无创、简单便捷、接受度高等特点,一直是疾病诊断领域研究的热点。
去年,剑桥大学的一家分支公司“欧尔斯通”开发了一台“肺癌显示检测器”,用于检查呼气中的化学物质,从而显示患者是否可能患有肺癌。包括来自利物浦大学一个小组的研究人员发现,细胞发出的气体有轻微的基因变异,他们认为利用呼气来诊断肺癌在理论上是可行的。
早在2010年,发表在英国《癌症》杂志上的一项研究中,以色列科学家就研发出了只要通过简单的呼吸测试,就可以查出罹患了肺、乳腺、肠和前列腺癌的病人的“电子鼻”。
这两年,英国剑桥大学的研究实验室也开发了一种“电子鼻”传感器。该传感器和美元的一角硬币(直径约1.8厘米)差不多大小,工作原理是制作出空气中化学物质的光谱,随后识别出每种化学物质的特殊构造。如果该传感器已经被设置,并校准到一个特定的水平,它就会拉响警报。
备注:本文根据合肥物质科学研究院以及Journal of Gastroenterology and Hepatology官网整理报道
原始出处:
[1] 医学物理中心发展食管癌筛查呼气质谱检测新方法
[2] Xue Zou,et al. Exhaled gases online measurements for esophageal cancer patients and healthy people by proton transfer reaction mass spectrometry. J Gastroenterology and Hepatololy. 23 November 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#GAS#
28
#诊断癌症#
22
#新突破#
27
#中科院#
31
#AST#
30
#EPA#
23