一文读懂:近期多发性硬化相关研究进展
2017-02-22 MedSci MedSci原创
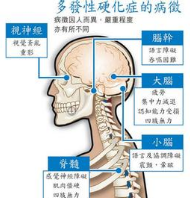
多发性硬化(Multiple Sclerosis,MS)是一种无法治愈的神经系统进展性疾病,主要损害脊髓、大脑以及视神经,易发于15-40岁青壮年人群,常见的症状有视力模糊、身体麻木、四肢异常疲劳等,如不治疗,严重时会造成突然失明、瘫痪。我国目前还缺乏这方面的流行病学数据,特点尚不明确。现在小M整理了关于MS研究的新进展及重大新闻与大家分享。【1】Neurology:新生儿维生素D缺乏与多发性
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#多发性#
40
#相关研究#
29
v刚刚黄河鬼棺天天
57
吃饭饭滚滚滚姑姑姑父发发发
66
#研究进展#
36
唱歌刚刚呵呵哈哈哈嘎嘎嘎
65
huthjunfaithful
60
好好努力
66
维生素D水平和多发性硬化症之间的相关性。
23
作为一名宝妈,希望这方面的研究越多越好
22