JNCI:重磅!科学家利用CRISPR/Cas9技术使癌症突变失活
2016-09-02 佚名 生物谷
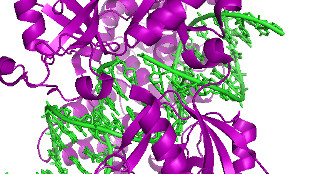
由于在许多生物医学和生物技术领域均有着广泛的应用,“基因魔剪”CRISPR/Cas9或将完全打开癌症研究领域的大门;日前一项刊登在国际杂志Journal of the National Cancer Institute上的研究报告中,来自德国德累斯顿工业大学 (Dresden University of Technology)等机构的研究人员通过研究发现,扮演癌症驱动子的突变或许能够被靶向作用并且
由于在许多生物医学和生物技术领域均有着广泛的应用,“基因魔剪”CRISPR/Cas9或将完全打开癌症研究领域的大门;日前一项刊登在国际杂志Journal of the National Cancer Institute上的研究报告中,来自德国德累斯顿工业大学 (Dresden University of Technology)等机构的研究人员通过研究发现,扮演癌症驱动子的突变或许能够被靶向作用并且修复,而且这些相关的突变也可以被快速诊断,并被用来改善个体化疗法。
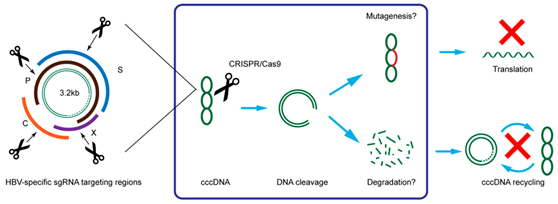
作为生物技术研究领域的革命性工具,CRISPR/Cas9在生物医学研究上有着其广泛的用途,其可以实现对细胞基因组中特定位点的DNA进行切割,如今研究人员就发现了一种方法,能够利用该技术诊断并且使得癌症突变失活,从而加速癌症领域的研究。研究者Frank Buchholz说道,通过新一代测序技术我们就能够快速鉴别出癌细胞中的突变,但很多时候我们并不知道到底是哪些突变能够驱动疾病的发生,而且哪些突变是相对良性的。
这项研究中,研究者首先对超过50万个报道的癌症突变进行分析,这些突变从理论上来讲能够被靶向作用,并且超过80%的突变都可以被CRISPR/Cas9系统进行切割修饰;随后研究者人员发现CRISPR/Cas9可以在不明显靶向作用健康野生型等位基因的同时,对一系列常见的癌症突变进行特异性靶向作用;此外,携带癌症特异性引导RNAs的Cas9酶类的表达还能够揭开引发癌细胞生长和变异的突变。
最后研究者Buchholz指出,这是一项重要的研究突破,因为如今我们可以从普通“乘客”突变中分裂出驱动癌症的突变,而这往往是癌症领域研究的薄弱环节,由于每一种癌症都会表现出特殊的突变组合,因此未来我们或许有可能开发出新型的手段来改善因突变促进癌细胞生长相关的癌症的诊断,当然本文研究仅仅是开始,后期研究人员还需要进行更为深入的研究来继续探索。
原始出处
Christina Gebler*, Tim Lohoff*, Maciej Paszkowski-Rogacz, Jovan Mircetic, Debojyoti Chakraborty, Aylin Camgoz, Martin V. Hamann, Mirko Theis, Christian Thiede and Frank Buchholz.Inactivation of Cancer Mutations Utilizing CRISPR/Cas9.JNCI.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CRISPR/Cas9技术#
46
#RISPR/Cas9#
51
#NCI#
38
后期研究人员还需要进行更为深入的研究来继续探索!
70
癌症的治疗可以,放疗~化疗~电疗~手术!
0
有些突变是良性!
71
#CRISPR#
31
#CRISPR/Cas9#
44
#Cas9#
41
#重磅#
27