Nat Med:科学家发现促进损伤后骨髓修复的方法
2018-01-19 MedSci MedSci原创
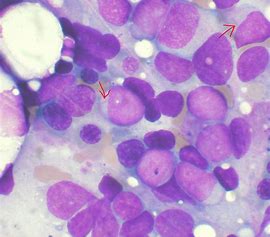
人类和小鼠的长周期自我更新造血干细胞(LT-HSCs)表达高水平的LH/绒毛膜促性腺激素受体(LHCGR),并且在LH刺激时这种受体会扩增。这个研究揭示了LH在调节HSC中的作用,并且为造血系统损伤后的造血恢复提供了新的治疗性方法。
骨髓毒性是大部分癌症治疗过程中普遍存在的副作用,并且是引起意外射线暴露者死亡的主要原因。因此,临床上对保护造血干细胞和以及由射线暴露造成的造血衰竭后的造血重建具有极大需求。但是目前还没有有效的治疗手段能够挽救射线损伤后的骨髓造血功能。
越来越多的研究表明性激素不仅能够促进性征的形成,并且能够调节造血干细胞的自我更新,分化和增殖。本研究者也曾报道过减少性类固醇能促进骨髓淋巴细胞的增殖以及老年和免疫耗尽的小鼠的骨髓恢复。因此,科学家发现促黄体生成激素(luteinizing hormone,LH)释放激素抑制剂(luteinizing hormone releasing hormone antagonist, LHRH-Ant)药物(目前在临床此药物广泛用为性激素抑制剂)能促进造血恢复,并且延长致死剂量全身照射的小鼠的存活时间。令人意外的是,这种保护效应并不依赖于性激素的作用,而是基于降低体内LH 的水平而获得的。
人类和小鼠的长周期自我更新造血干细胞(LT-HSCs)表达高水平的LH/绒毛膜促性腺激素受体(LHCGR),并且在LH刺激时这种受体会扩增。这个研究揭示了LH在调节HSC中的作用,并且为造血系统损伤后的造血恢复提供了新的治疗性方法。
文章出处:Velardi E, Tsai J J, Argyropoulos K V, et al. Suppression of Luteinizing Hormone Enhances HSC Recovery after Hematopoietic Injuries[J]. 2016.
本文由梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Nat#
29
#科学家发现#
30
#损伤#
26
#Med#
21