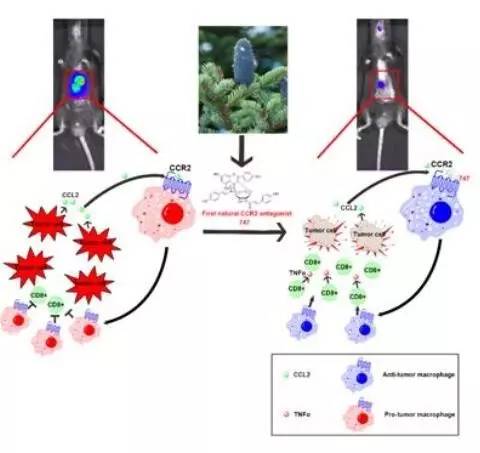
EBioMedicine:研究人员发现新型天然小分子调节免疫重塑肿瘤微环境治疗肝癌
2017-08-09 佚名 中科院之声
近日,《细胞》出版社和《柳叶刀》杂志联合支持的 EBioMedicine 杂志在线发表了中国科学院上海生命科学研究院(人口健康领域)王慧组的研究论文 A Natural CCR2 Antagonist Relieves Tumor-associated Macrophage-mediated Immunosuppression to Produce a Therapeutic Effect for
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CIN#
28
#研究人员#
35
#小分子#
25
#Bio#
23
#DIC#
24
#Medicine#
28
#Med#
20
#EBI#
18
学习学习学习
61