Cancer Gene Ther:GLUT1基因在膀胱泌尿道上皮细胞癌中的多态性分析以及与p53、Ki67和GLUT1表达的关系
2017-05-23 AlexYang MedSci原创
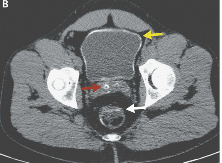
最近,有研究人员就两个葡萄糖载体1(GLUT1)在膀胱泌尿道上皮细胞癌(UCC)患者和204名正常人中的单核苷酸多态性(SNPs)(XbaI G>T 和 HaeIII T>C)进行了研究分析。研究人员利用免疫组化实验评估了p53、Ki67和GLUT1的表达情况。研究发现,TT基因型的频率和XbaI G>T的T等位基因SNP频率在膀胱泌尿道上皮细胞癌病人中降低了。CC基因型的频率和
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#细胞癌#
33
#GLUT1#
0
#Gene#
25
#尿道#
24
#p53#
29
#上皮细胞#
25
#多态性#
24