JCI insight:能透析的人工肾脏问世
2016-06-10 药明康德 MedSci原创
近日,发表在《JCI insight》期刊上的一项探索性临床实验结果表明,便携式的人工肾脏可能成为一种可行的新透析技术。这项技术可能给予晚期肾病患者传统血液透析以外的另一个选择。 目前,对晚期肾病患者的治疗方法是进行血液透析。这需要患者每周三天与血液透析机连接接受治疗。当患者接受血液透析时,由于透析机是固定的,患者的活动能力在接受治疗时非常有限。长期以来,接受透析的患者和他们的家属非常希望这
近日,发表在《JCI insight》期刊上的一项探索性临床实验结果表明,便携式的人工肾脏可能成为一种可行的新透析技术。这项技术可能给予晚期肾病患者传统血液透析以外的另一个选择。
目前,对晚期肾病患者的治疗方法是进行血液透析。这需要患者每周三天与血液透析机连接接受治疗。当患者接受血液透析时,由于透析机是固定的,患者的活动能力在接受治疗时非常有限。长期以来,接受透析的患者和他们的家属非常希望这个过程能够在家里进行,并且在接受透析时能够有更多的独立性和行动上的自由。
一个能够让患者佩戴的透析机能够让患者不被栓在一个地方,给他们更多的活动自由。同时,便携式的透析机还能给患者提供其它益处,包括更长时间或更频繁的透析治疗。为此,美国FDA于2015年秋天批准在西雅图的华盛顿大学医学中心(University of Washington Medical Center)进行了一项对便携式人工肾脏样机的临床实验。这项实验力图确定样机的安全性和有效性。同时,研究人员听取了患者对这种实验性疗法的反响。
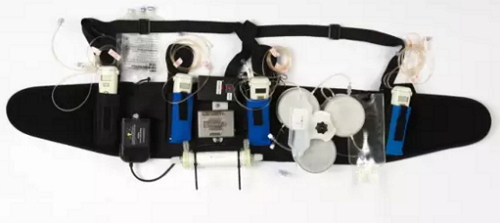
便携式人工肾脏
总计有7名患者接受了便携式人工肾脏的治疗。患者佩戴仪器的时间可长达24小时。实验结果表明,便携式人工肾脏可以有效地清除血液中的代谢废物,包括尿素,肌酐,磷,并且去除多余的水分和盐分。这些都是正常肾脏能够行使的功能。当患者接受传统透析治疗时,他们的饮食通常有很强的局限性。与之相比,这些佩戴人工肾脏的患者在实验过程中即使没有任何饮食方面的限制,他们血液中的电解质(例如钠离子和钾离子)水平, 和血液中的液体容量都能够保持平衡。调节体液的容量和成份也是正常肾脏的功能之一。
在临床实验过程中,患者对人工肾脏的耐受性良好,没有很严重的副作用产生。而且参与实验的病人都表示,与传统的在透析中心接受治疗相比,这种新疗法更令人满意。“它对我的效果这么好让我很吃惊。虽然这个仪器有些笨重,但是如果今天让我选择的话我还是会选择使用它。它给了我好多自由。”参与实验的一位患者, Chuck Lee说。
根据临床实验的结果,研究人员将进一步改善便携式人工肾脏的设计,着重于让它的使用更加方便和增强仪器运作的可靠性。最终的目标是让这台设备能够在家里被病人或他们的护理人员独立操作。
原始出处
Victor Gura,1,2 Matthew B. Rivara,3 Scott Bieber,3 Raj Munshi,3,4 Nancy Colobong Smith,3,5 Lori Linke,3 John Kundzins,3 Masoud Beizai,6 Carlos Ezon,6 Larry Kessler,3,7 and Jonathan Himmelfarb3.A wearable artificial kidney for patients with end-stage renal disease.JCI insight
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#人工肾#
32
#JCI#
25
会越来越精巧
92
这个厉害
92
科学进步
147