美国医生呼吁:左心耳封堵术应终止,其预防卒中的作用有限
2016-11-25 文韬 中国循环杂志
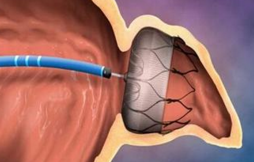
近期美国临床电生理医生John Mandrola 在Medscape撰文称,“左心耳封堵治疗以预防非瓣膜性房颤(AF)患者中风可能是心脏病学的一个错误。” John Mandrola认为,左心耳封堵不能预防缺血事件。因为根据常识,中风是一种系统性疾病,封堵左心耳仅仅是一个方面。在房颤患者中,心血管危险因素、可致中风的非房颤机制和基质也会增加中风风险。 而且,根据目前的随机对照临
近期美国临床电生理医生John Mandrola 在Medscape撰文称,“左心耳封堵治疗以预防非瓣膜性房颤(AF)患者中风可能是心脏病学的一个错误。”
John Mandrola认为,左心耳封堵不能预防缺血事件。因为根据常识,中风是一种系统性疾病,封堵左心耳仅仅是一个方面。在房颤患者中,心血管危险因素、可致中风的非房颤机制和基质也会增加中风风险。
而且,根据目前的随机对照临床研究,用Watchman封堵左心耳预防缺血性中风并未优于华法林。John Mandrola的主要观点如下:
PROTECT-AF试验比较了房颤患者中的Watchman和华法林(平均CHA2DS2-VASc = 3.5)的效果。该研究证实尽管证实,Watchman包括中风、心血管死亡和全身性栓塞的复合主要终点不劣于华法林。但FDA仍担心其并发症,认为如果左心耳封堵有效,应该减少缺血性中风和全身性栓塞。然而,Lancet对PROTECT-AF回顾分析显示,Watchman组的缺血性中风和全身性栓塞的发生率高出50%(17/463 vs 6/244)。而且这还是在15%的患者在坚持抗凝的情况下。FDA要求进行另一个试验。
五年后,在2014年7月,PREVAIL研究公布,该研究比较了407名高风险房颤(平均CHA2DS2-VASc= 3.8)患者中Watchman和华法林。并设定了三个复合终点:安全性,主要疗效和晚期缺血性疗效终点(主要是排除了植入后第一周的事件)。
Watchman组终点下降到2.2%,远低于PROTECT-AF研究的7.4/100人年。对于PREVAIL的第一主要疗效终点,出血性或缺血性中风、全身性栓塞和心血管/未解释的死亡事件率的复合终点相似(6.4%对6.3%),未达到劣效标准。即Watchman劣于标准治疗。在Watchman组中,269个患者中有6个缺血性卒中或全身性栓塞,而在对照组中的138个患者中仅有一个。
2014年7月,JACC发表了PREVAIL研究,只有28%患者达到18个月的随访期,缺血性卒中或全身性栓塞的晚期事件发生率为2.5%,对照组中为2.0%。这一结果达到Watchman不劣于华法林的统计标准。
但在TCT 2014年会议上和2014年10月在第三次FDA听证会上,PREVAIL的长期数据中,Watchman组新发了8个缺血性卒中。这样Watchman组就有了13个缺血事件,而在对照组中仅有一个缺血事件。有了这个更新的数据,Watchman就没有达到非劣效标准。
而在2015年发表在JACC杂志患者水平的Meta分析中,虽然出血性中风和全因中风或全身性栓塞的复合终点非劣效发生率较低。但是,Watchman组缺血性卒中发生频率几乎增加一倍(HR=1.95,P=0.05)。值得注意的是,第三次FDA咨询会上多数人不相信Watchman有效。
John Mandrola 指出,PREVAIL研究的长期随访结果表明,Watchman未优于华法林。但有影响力的心血管科医生仍在引用不完整的PREVAIL论文。例如,新的2016年ESC房颤治疗指南援引PROTECT AF和不完整的2014 PREVAIL论文,说Watchman不劣于华法林。来自一位德国和两位美国作者的另一篇2016年评论文章也称Watchman不劣于华法林,同样参考了JACC的PREVAIL论文。
原始出处:
1、Medcape:Left Atrial Appendage Closure Should Stop now.
2、John Mandrola 的博客:Say No to Watchman
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#封堵术#
34
#左心耳封堵术#
44
#左心耳#
37
#美国医生#
57
才听说还有这功能
57
才听说
59