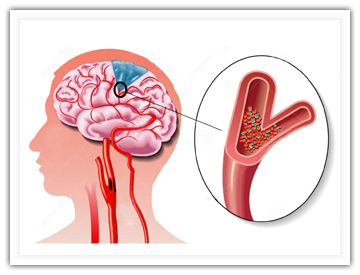
Stroke:对于TIA患者,那些扑朔迷离的非典型临床症状!
2017-06-14 shaosai MedSci原创
相对于典型的一过性缺血症状(TS),非典型的短暂性脑缺血症状主要包括部分感觉缺失、构音障碍、眩晕或不稳,少见的皮层性视觉障碍和复视。当这些症状单独发生时,临床医生往往不能将此归类于短暂性脑缺血发作(TIA)的临床症状,同时,该种情况的临床发生率尚不明确。本研究纳入了2003-2008年间短暂性脑缺血发作临床中心收治的典型的TIA患者,并对颅脑、动脉及心脏进行了系统的检查。在排除主要鉴别诊断之后,研
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TIA患者#
37
#临床症状#
31
好好学习,涨知识
61
#非典型#
38