J Cell Biol:樊代明院士发现miR-7可抑制胃癌的发展
2015-08-12 sunshine 译 MedSci原创
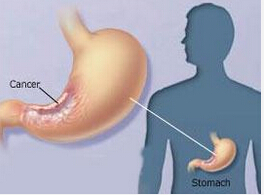
据发表于Cell Biology 的一项研究表明,Cell Biology miR-7可通过抑制一个关键的信号通道以抑制胃癌的发生,而且这种保护机制可被致癌细菌幽门螺杆菌所损害。因此,发现能够诱导miR-7的药物可因此成为抑制胃癌发展的一项有效的治疗手段。据美国国立卫生研究院称,胃癌是全球第四大常见的癌症,且是癌症相关死亡的第三大原因。常在胃癌中表达降低的miR-7可通过抑制特定生长因子受体(IG
据发表于J Cell Biology 的一项研究表明,Cell Biology miR-7可通过抑制一个关键的信号通道以抑制胃癌的发生,而且这种保护机制可被致癌细菌幽门螺杆菌所损害。
因此,发现能够诱导miR-7的药物可因此成为抑制胃癌发展的一项有效的治疗手段。
据美国国立卫生研究院称,胃癌是全球第四大常见的癌症,且是癌症相关死亡的第三大原因。常在胃癌中表达降低的miR-7可通过抑制特定生长因子受体(IGF1R)阻止癌细胞扩散至其他组织。然而,miR-7是否也可抑制胃癌的早期阶段尚未可知,因此中国的研究员筛查了microRNA的新靶点。
Dai-Ming Fan及其同事发现miR-7的直接靶向基因-RELA 及FOS基因,该基因可分别编码参与原癌基因NF-κB 及AP-1信号通路的蛋白质。在人类胃癌标本中,低水平的miR-7与RELA及FOS蛋白的水平升高及患者生存率较低有关。小鼠实验研究发现,miR-7的水平升高可降低RELA 及FOS的水平并抑制肿瘤生长。
研究人员发现,除可直接抑制RELA的表达外,miR-7还可通过在NF-κB信号通路中靶向作用于其上游激酶(IKKε)以控制蛋白质的活化。然而,这一相同的通路本身可抑制miR-7的表达,表明了如果NF-κB通路被强烈激活,那么miR-7将无法抑制RELA的活性。
慢性幽门螺旋杆菌感染是胃癌发生的主要危险因素,部分是由于该细菌可以过度激活NF-κB通路。因此,Fan及其同事发现将幽门螺旋杆菌与胃细胞共同培养可激活IKKε及RELA,并减少miR-7的表达,这是正常胃细胞转化为癌细胞关键步骤。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
28
#Bio#
23
#miR#
30
希望能研制出这种药,来为临床再做贡献,
144
希望能研制出这种药,来为临床再做贡献,
120
赞!
106
赞!
67
嗯,好消息,
129
嗯,好消息,
52
#Biol#
20