ACR:代谢综合征可增加原发性抗磷脂综合征患者发生动脉事件的风险
2012-11-29 Arthritis Care & Res Arthritis Care & Res
代谢综合征是原发性抗磷脂综合征病人发生动脉事件的一个独立危险因素在全世界范围内,代谢综合征(MetS)是一个主要的公共卫生问题。据报道,在原发性抗磷脂综合征(APS)病人中,MetS的发病率也很高。由于MetS和APS在引起内皮细胞功能障碍和增加血栓形成上有相似性,使得2种疾病共存的病人的表现可能不同也可能加重。目前此类文献报道仅有一例且APS病人的MetS发病率高。针对这种情况来自巴西圣保罗大学
代谢综合征是原发性抗磷脂综合征病人发生动脉事件的一个独立危险因素
在全世界范围内,代谢综合征(MetS)是一个主要的公共卫生问题。据报道,在原发性抗磷脂综合征(APS)病人中,MetS的发病率也很高。由于MetS和APS在引起内皮细胞功能障碍和增加血栓形成上有相似性,使得2种疾病共存的病人的表现可能不同也可能加重。目前此类文献报道仅有一例且APS病人的MetS发病率高。针对这种情况来自巴西圣保罗大学的Rodrigues CE等研究人员进行了一项研究来评价MetS在原发性APS病人中的临床显著性,研究结果发表在2012年10月的《关节炎治疗与研究》(Arthritis Care & Research)杂志上。研究发现,MetS可以增加APS病人患动脉事件的风险。
该研究为一项回顾性横断面研究。本研究共入组71例原发性APS患者和73例年龄与性别相匹配的健康对照。血浆样本用来测定血脂、Lp(a)、葡萄糖、胰岛素、促甲状腺激素、游离T4、红细胞沉降率、C反应蛋白和尿酸。应用国际糖尿病联合会标准确诊MetS,并使用稳态模型评价指标确定胰岛素抵抗。
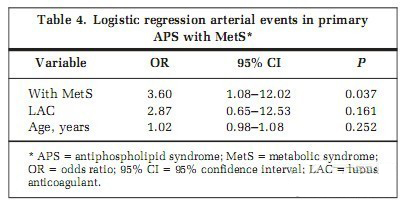
研究结果发现,MetS发病率为33.8%,对原发性APS病人继发性APS病人的进一步比较揭示前者有更高发生频率的动脉事件 (79.2% 比42.6%; P= 0.003)、心绞痛(29.2% 比 2.1%; P=0.002)和阳性狼疮抗凝抗体(95.8% 比76.6%; P=0.049)。另外,有MetS的原发性APS患者,正如预期那样,有更高的心血管发病率危险因素。多变量分析显示,在原发性APS中只有MetS与动脉事件独立相关(p=0.037)。
研究结果表明,原发性APS与MetS共存似乎可以鉴别有更高动脉事件风险的病人亚群。MetS可能会加重已经存在的原发性APS的内皮异常状态。

Objective
Metabolic syndrome (MetS) is highly prevalent in rheumatic diseases and is recognized as a new independent cardiovascular risk factor. This study was undertaken to determine the clinical significance of MetS in patients with primary antiphospholipid syndrome (APS).
Methods
Seventy-one primary APS patients and 73 age- and sex-matched healthy controls were included. Serum samples were tested for lipid profile, Lp(a), glucose, insulin, thyroid-stimulating hormone, free T4, erythrocyte sedimentation rate, C-reactive protein level, and uric acid. MetS was defined by the International Diabetes Federation criteria, and insulin resistance was established using the homeostasis model assessment index.
Results
The prevalence of MetS was 33.8%, and further comparison between primary APS patients with and without MetS revealed that the former had a higher frequency of arterial events (79.2% versus 42.6%; P = 0.003), angina (29.2% versus 2.1%; P = 0.002), and positive lupus anticoagulant antibody (95.8% versus 76.6%; P = 0.049). In addition, primary APS patients with MetS, as expected, had a higher prevalence of cardiovascular risk factors. On multivariate analysis, only MetS was independently associated with arterial events in primary APS.
Conclusion
Coexistence of primary APS and MetS seems to identify a subgroup of patients with higher risk of arterial events, suggesting that MetS may aggravate existing endothelial abnormalities of primary APS.
全文下载:
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#原发性#
45
#ACR#
26
#综合征#
44