European Radiology:I期肺癌的术前穿刺活检技术与同侧胸膜复发的关系
2022-04-06 shaosai MedSci原创
胸膜复发是PTNB的一种罕见的、潜在的长期并发症。在术前PTNB后接受早期肺癌治愈性切除的患者中,同侧肺癌的胸膜复发频率高于未接受PTNB的患者,这是一个值得关注的问题。
 由于低剂量计算机断层扫描(CT)筛查早期肺癌的普及,肺结节的发现率显著提高。当CT图像上检测到结节时,处理原则取决于恶性肿瘤的风险,对有肺癌风险的结节进行病理诊断对于指导适当的治疗至关重要。经皮经胸针刺肺活检(PTNB)被广泛用于肺癌的病理诊断,诊断肺癌提供了较高的准确性。PTNB最常见的并发症是气胸,其次是咯血和肺出血。
由于低剂量计算机断层扫描(CT)筛查早期肺癌的普及,肺结节的发现率显著提高。当CT图像上检测到结节时,处理原则取决于恶性肿瘤的风险,对有肺癌风险的结节进行病理诊断对于指导适当的治疗至关重要。经皮经胸针刺肺活检(PTNB)被广泛用于肺癌的病理诊断,诊断肺癌提供了较高的准确性。PTNB最常见的并发症是气胸,其次是咯血和肺出血。
胸膜复发是PTNB的一种罕见的、潜在的长期并发症。在术前PTNB后接受早期肺癌治愈性切除的患者中,同侧肺癌的胸膜复发频率高于未接受PTNB的患者,这是一个值得关注的问题。众所周知,胸膜复发的危险因素取决于肺癌的特点,包括体积较大、胸膜下位置、伴有脏层胸膜浸润或病理检查中的微小淋巴侵犯。如果术前PTNB与胸膜复发的发生有关,那么一些程序因素可能会影响胸膜复发的风险,但临床上缺少对这种因素的相关研究。
近日,发表在European Radiology杂志的一项研究探讨了特定的PTNB技术是否会降低I期肺癌治愈性切除术后同侧胸膜复发的风险,为该技术的进一步广泛应用铺平了道路。
本研究回顾性地纳入了415名从2009年到2016年连续接受术前PTNB和治愈性切除的I期肺癌患者,并收集了详细的信息,包括肺癌的临床、PTNB技术、放射学和病理学特征。进行Cox回归分析以确定倾向性评分匹配前后胸膜复发的风险因素。
PTNB后的总随访期为62.1±23.0个月,40名患者发生同侧胸膜复发。在倾向评分匹配前,年龄(p = 0.063)、显微镜下胸膜侵犯(p = 0.065)和病理肿瘤大小(p = 0.016)在单变量分析中倾向于与胸膜复发相关,随后使用倾向评分进行匹配。倾向评分匹配后,多变量分析显示,同侧胸膜复发与CT的目标尺寸较大(危险比[HR]=1.498;95%CI,1.506-2.125;p=0.023)和显微镜下淋巴侵犯(HR=3.526;95%CI,1.491-8.341;p=0.004)有关。然而,没有任何PTNB技术,如针距、活检或胸膜通道数与复发风险的降低有关。
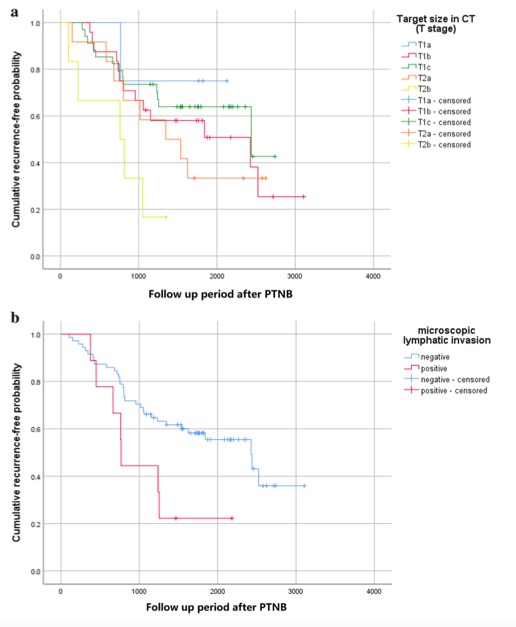
图 根据(a)计算机断层扫描(CT)上的目标尺寸和(b)显微镜下的淋巴侵犯,倾向评分匹配后的无复发生存率的Kaplan-Meier图。
总之,在使用PSM调整肿瘤和患者特征后,没有特定的PTNB技术可以减少I期肺癌PTNB后的同侧胸膜转移。无论采用何种具体技术,当怀疑是早期肺癌时,需要谨慎地应用PTNB,然后进行根治性手术治疗。
原文出处:
Min Gwan Kim,Bo Ram Yang,Chang Min Park,et al.Preoperative percutaneous needle lung biopsy techniques and ipsilateral pleural recurrence in stage I lung cancer.DOI:10.1007/s00330-021-08359-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#胸膜#
56
#PE#
45
#穿刺活检#
66
学习了。
55
#活检#
50
#穿刺#
50