曲安奈德联合抗VEGF药物球内注射治疗脉络膜结核瘤1例
2018-04-17 惠巧艳 李晶明 郭省香 临床眼科杂志
患者男性,18岁。因左眼视力下降伴视物变形1个月就诊,
【一般资料】
患者男性,18岁。
【主诉】
因左眼视力下降伴视物变形1个月就诊,
【既往史】
无眼痛眼胀、恶心呕吐,有肺结核病史。
【体格检查】
右眼视力1.0,左眼视力0.02,矫正不提高,右眼眼压:13mmHg左眼眼压:12mmHg,双眼屈光间质清,右眼眼底未见明显异常,左眼眼底视盘色淡红,边界清楚,C/D=0.2,黄斑中心凹上方可见一直径约2PD大小的黄白色病灶,呈半球形隆起状,周围有渗出,水肿明显,中央可见斑点状色素沉着及少量点状出血点,病灶下方5~8点及上方10~12点处周边部视网膜呈放射状皱褶样改变,波及黄斑区,黄斑水肿明显,中心凹反射不清(图1A,1B)。
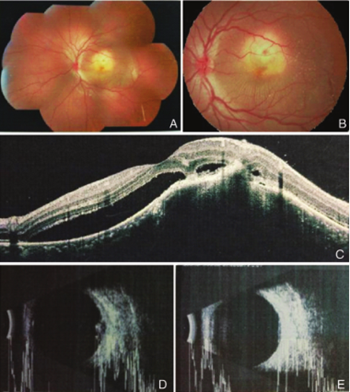
图1 治疗前:A、B:黄斑中心凹上方 2PD的黄白色隆起病灶,中央色素沉着及点状出血,病灶下方5-8点及10-12点处周边视网膜呈放射状皱褶改变;C:黄斑区视网膜隆起伴神经上皮层脱离,少量神经上皮层间水肿,脱离的神经上皮与色素上皮之间是低反射液性区:D、E:视盘颞侧脉络膜局限低回声隆起,继发性视网膜脱离
【辅助检查】
B超检查示:视盘颞侧脉络膜局限性低回声隆起,继发性视网膜脱离(图1D,1E)。应用相干光断层成像术(OCT)黄斑部扫描示:黄斑区视网膜隆起伴神经上皮层脱离,合并少量神经上皮层间水肿,脱离的神经上皮与色素上皮之间是低反射的液性区(见图1C)。荧光素眼底血管造影FFA示:早期黄斑上方约1.5PD大小的环形强荧光区,中央色素遮蔽荧光,晚期强荧光区荧光强度逐渐增强,略向周围扩大,边界较清楚(图2A~C)。吲哚青绿眼底血管造影(ICGA)示:早期黄斑上方约2PD大小的低荧光病灶,中晚期病灶内持续低荧光,边界不清楚,周围散在的低荧光点状病灶(图2D~F)。
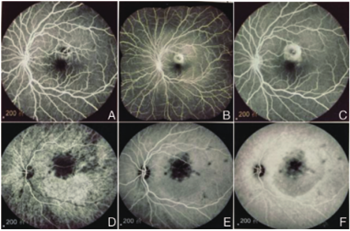
图2 治疗前:FFA(A、B、C)示:早期黄斑上方约 1.5 PD的环形强荧光区,中央色素遮蔽荧光,晚期强荧光区荧光强度逐渐增强,略向周围扩大,界清;ICGA(D、E、F)示:早期黄斑上方2 PD的低荧光病灶,中晚期持续低荧光,界不清,周围散在的低荧光点状病灶
【初步诊断】
结合病史、体征和辅助检查诊断为左眼脉络膜结核瘤。
【治疗】
在全身抗结核治疗下加用球结膜下注射链霉素0.3g,隔日1次,持续治疗1个月后左眼视力指数/10cm,治疗效果不佳,遂停用球结膜下注射链霉素,改为玻璃体腔注射曲安奈德2mg和贝伐珠单抗1.25mg,约5周1次,同时预防性给予噻吗洛尔滴眼,2次/日,卡林-U滴眼,3次/日,降低眼压升高及并发性白内障发生的风险。持续治疗10个月后左眼视力恢复至0.8,矫正视力1.0,眼底见黄斑中心凹上方黄白色局限隆起病灶,边界清楚,周围无渗出及水肿,中心凹反光存在。复查OCT示:左眼黄斑区视网膜局限隆起,渗出性神经上皮层脱离和神经上皮层间水肿完全消失(见图3A,3B)。定期治疗随访1年余,视力稳定。
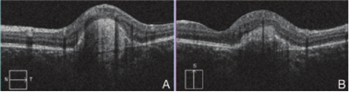
图3 治疗后:OCT(A、B)示:黄斑区视网膜局限隆起,渗出性神经上皮层脱离和神经上皮层间水肿完全消失
【讨论】
该患者有明确的肺结核病灶及典型的眼底表现,结合其抗结核治疗有效,诊断明确。脉络膜结核瘤大多数继发于全身其他部位的结核感染,主要是由于结核杆菌经血源播散所致。脉络膜血流缓慢,血管丰富,结核杆菌容易滞留此处而发生感染。结核杆菌毒素对组织的直接毒性损害和脉络膜组织对结核菌体蛋白的变态反应同时作用引起组织炎症反应。其治疗主要采用全身抗结核,常多种药物联合使用。有临床和实验证明,在使用抗结核药物的同时,全身加用低剂量肾上腺糖皮质激素会减轻超敏反应引起的组织损伤。因此为了减轻该患者脉络膜组织损害,在口服抗结核药物治疗下,加球内注射糖皮质激素,且全身使用抗结核药物有效避免单用激素促使结核杆菌繁殖扩散而引发感染加剧。该患者脉络膜炎症反应较重,联合使用抗VEGF药物抑制新生血管的生成,减轻组织水肿。
原始出处:
惠巧艳, 李晶明, 郭省香,等. 曲安奈德联合抗VEGF药物球内注射治疗脉络膜结核瘤1例[J]. 临床眼科杂志, 2017, 25(4):378-379.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#曲安奈德#
52
#结核瘤#
33
#脉络膜#
32
学习了.第一次看到
71
#结核#
47
#VEGF#
34
#抗VEGF#
47