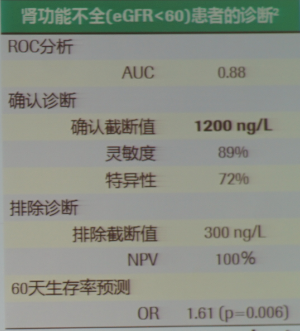
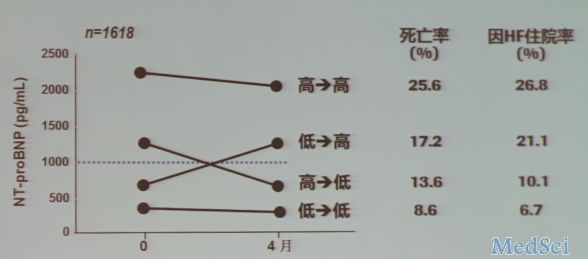
CIHFC 2016:张宇辉:中国心衰诊疗的现状及NT-proBNP的临床应用(下)
2016-03-17 小M MedSci原创
当今世界上最好的心血管医生Eugene Braunwald教授曾评价:心力衰竭是心脏病最后的战场。心衰是一个与时俱增的疾病,随着年龄的增长,心衰的发病率也会逐渐增高,而当今世界处于一个全球老龄化的状态中,因此临床医生需要更深入地认识与诊治心衰。那么中国心衰诊疗的现状是怎样的呢? 3月12日,在中国国际心力衰竭大会新闻发布会上,来自中国医学科学院阜外医院心力衰竭中心的本届大会秘书长、张
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#临床应用#
36
值得学习
125
好,值得学习。
88
#BNP#
36
#NT-proBNP#
44
#PRO#
32
感谢分享。
139
指标
100