典型病例:生命的“恶魔”碰到“郗奇”的医生
2018-07-15 柴潇 中国军网综合
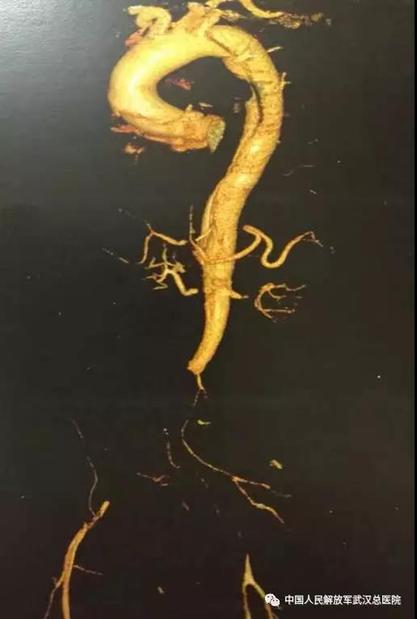
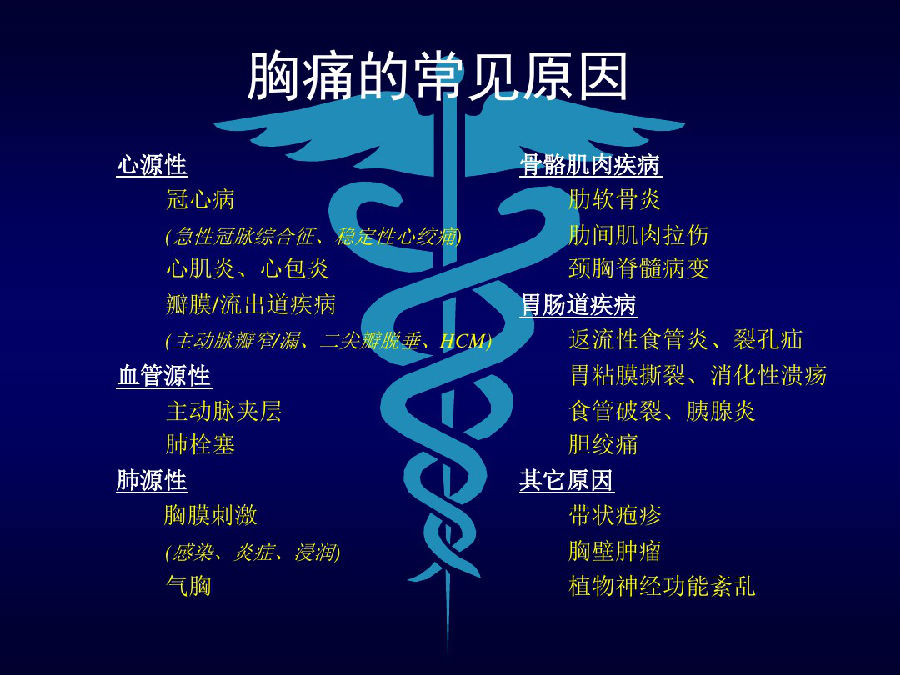
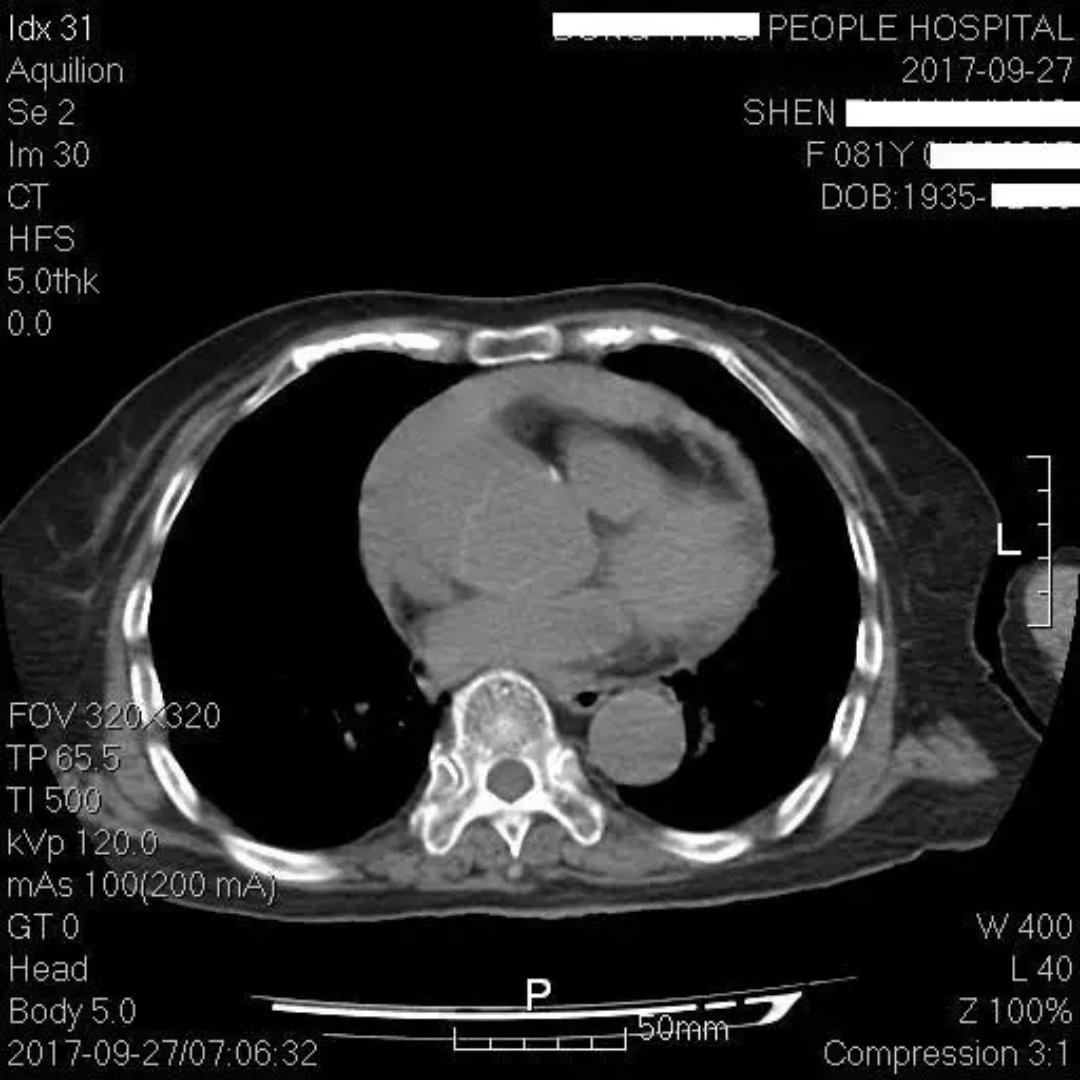
近日,解放军武汉总医院心胸外科收治了几例主动脉夹层合并肠缺血(灌注不良)的患者。这到底是一种什么病?又有多危险呢?请随走过“鬼门关”的郑先生来了解下!

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了,谢谢分享
55
好文献学习了
52
好文献学习了
0
学习了.涨知识了!
50
好
64
了解一下.谢谢分享!
20