Radiology:输尿管口膀胱肿瘤的多参数MRI评价
2022-09-15 shaosai MedSci原创
为了规范多参数MRI和膀胱癌的影像学报告,2018年5月临床引入了膀胱成像报告和数据系统(VI-RADS)。
 据统计,膀胱癌是最常见的泌尿系统恶性肿瘤,具有较高的复发率。膀胱癌的临床治疗取决于肌肉侵犯的状况。非肌肉浸润性膀胱癌(NMIBCa)通常等级较低,治疗方法是经尿道切除膀胱肿瘤。相比之下,肌肉浸润性膀胱癌(MIBCa)是一种侵袭性肿瘤,预后较差,常需要根治性膀胱切除术、化疗、放疗或两者结合。随着MRI技术的快速发展,多参数MRI已成为经尿道切除膀胱肿瘤的重要补充工具。为了规范多参数MRI和膀胱癌的影像学报告,2018年5月临床引入了膀胱成像报告和数据系统(VI-RADS)。在T2加权成像、弥散加权成像和动态对比增强成像的基础上,VI-RADS以五分法的方式预测膀胱癌肌肉浸润的可能性。众多研究表明,VI-RADS是检测MIBCa 0的有效综合评估手段。
据统计,膀胱癌是最常见的泌尿系统恶性肿瘤,具有较高的复发率。膀胱癌的临床治疗取决于肌肉侵犯的状况。非肌肉浸润性膀胱癌(NMIBCa)通常等级较低,治疗方法是经尿道切除膀胱肿瘤。相比之下,肌肉浸润性膀胱癌(MIBCa)是一种侵袭性肿瘤,预后较差,常需要根治性膀胱切除术、化疗、放疗或两者结合。随着MRI技术的快速发展,多参数MRI已成为经尿道切除膀胱肿瘤的重要补充工具。为了规范多参数MRI和膀胱癌的影像学报告,2018年5月临床引入了膀胱成像报告和数据系统(VI-RADS)。在T2加权成像、弥散加权成像和动态对比增强成像的基础上,VI-RADS以五分法的方式预测膀胱癌肌肉浸润的可能性。众多研究表明,VI-RADS是检测MIBCa 0的有效综合评估手段。
然而据报道,VI-RADS标准也有一定的局限性,特别是对于位于输尿管口的肿瘤来说最为明显。据报道,对于发生在输尿管口的肿瘤来说,VI-RADS评分的观察者间一致性较差。近日,发表Radiology杂志的一项研究探讨了VI-RADS在评估位于输尿管口的膀胱肿瘤的肌肉侵犯方面的诊断性能和观察者间的一致性,为VI-RADS的进一步广泛应用提供了数据支持。
本项回顾性研究收集了2012年1月至2021年11月期间发生在输尿管口的组织病理学证实的膀胱癌患者。两位放射科医生使用盲法根据VI-RADS对多参数MRI扫描进行了独立评分。使用加权κ分析评估了VI-RADS评分的观察者间一致性。使用过ROC分析评估VI-RADS评分在预测肌肉侵犯方面的诊断性能。
共有78名患者(平均年龄,67岁±7[SD];年龄范围,46-90岁;67名男性)纳入最终分析:25名非肌肉浸润性膀胱癌患者和53名肌肉浸润性膀胱癌(MIBCa)患者。在共识阅读时,1例(1%)被打为VI-RADS 1,27例(35%)被打为VI-RADS 2,6例(8%)被打为VI-RADS 3,10例(13%)被打为VI-RADS 4,34例(44%)被打为VI-RADS 5。在将VI-RADS评分与组织病理学结果进行比较时,证实VI-RADS 1的肌肉侵犯存在率为0%(1中0),VI-RADS 2为15%(27中4),VI-RADS 3为83%(6中5),VI-RADS 4为100%(10中10),而VI-RADS 5为100%(34中34)。VI-RADS检测MIBCa的AUC为0.96(95%CI:0.92,1.00)。
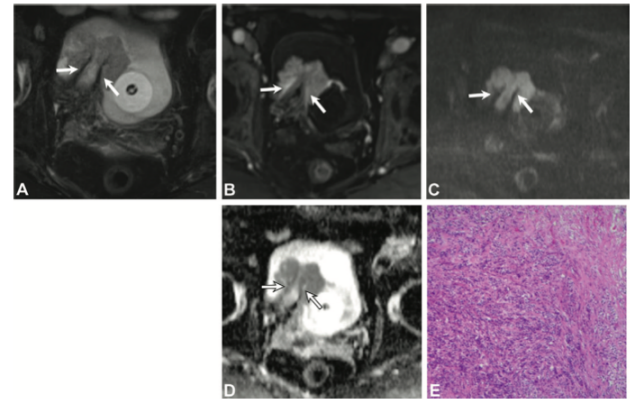
图 一位67岁的男性患者,患有pT2低分级尿路上皮癌。(A) 轴位T2加权图像显示右输尿管口上方肿瘤,伴有输尿管积水。表现为高信号的增厚内壁显示不清,但低信号的固有肌层(箭头)显示尚清。(B) 轴位对比增强图像显示内壁的早期增强(箭头)。(C) 弥散加权和(D)表观弥散系数图像显示肿瘤和膀胱壁之间的低信号(箭头)。所有读者的最终膀胱成像报告和数据系统评分为2分。(E) 膀胱部分切除术后获得的组织病理学图像显示逼尿肌受侵。(血红蛋白染色;原始放大倍数,3100)
本研究结果表明,位于输尿管口的膀胱癌有较高的逼尿肌侵犯情况。此外,膀胱成像报告和数据系统的评分系统可用于肌肉浸润性膀胱癌的准确预测及评估。
原文出处:
Qian Cai,Jian Ling,Lingmin Kong,et al.Multiparametric MRI Evaluation of VI-RADS for Bladder Tumors Located at the Ureteral Orifice.DOI:10.1148/radiol.220028
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#输尿管#
48
#膀胱肿瘤#
40
学习了
33
#评价#
51
学习
33