芝加哥肺科医生马丁 托宾(Martin Tobin)
上周四,专攻肺部和呼吸的著名医学专家马丁·托宾博士在前军官德里克·肖文(Derek Chauvin)的谋杀案审判中作证时说,乔治·弗洛伊德因呼吸浅而死于低氧。遭受弗洛伊德先生如此行为的健康人也可导致死亡,法医解剖可见大脑造成了损害,并且还引起了 PEA心律失常导致他的心脏停止跳动。
他补充说:“低氧的原因是呼吸浅,小呼吸。潮气量小,浅呼吸无法将空气通过肺部输送到肺的基本区域,从而使氧气进入血液并消除二氧化碳。”
托宾用容易理解的语言解释医学概念,甚至松开领带以说明观点,托宾告诉陪审团说,弗洛伊德的呼吸受到严重限制,而乔文和另外两名明尼阿波利斯官员将这位46岁的黑人压在了他的身上。 目击者称,缺氧导致大脑受损,并使他的心脏停止。
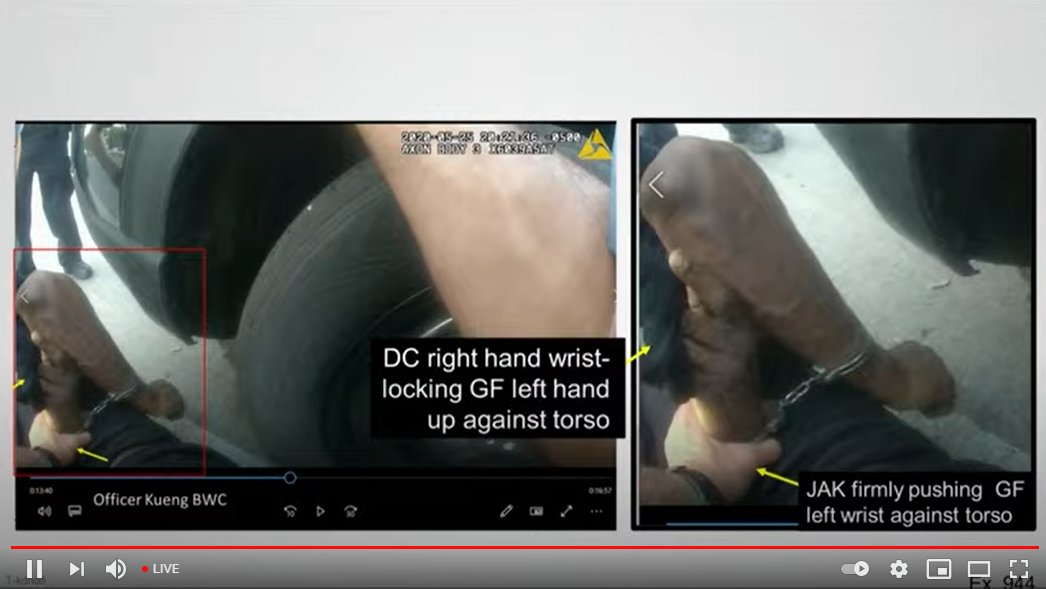
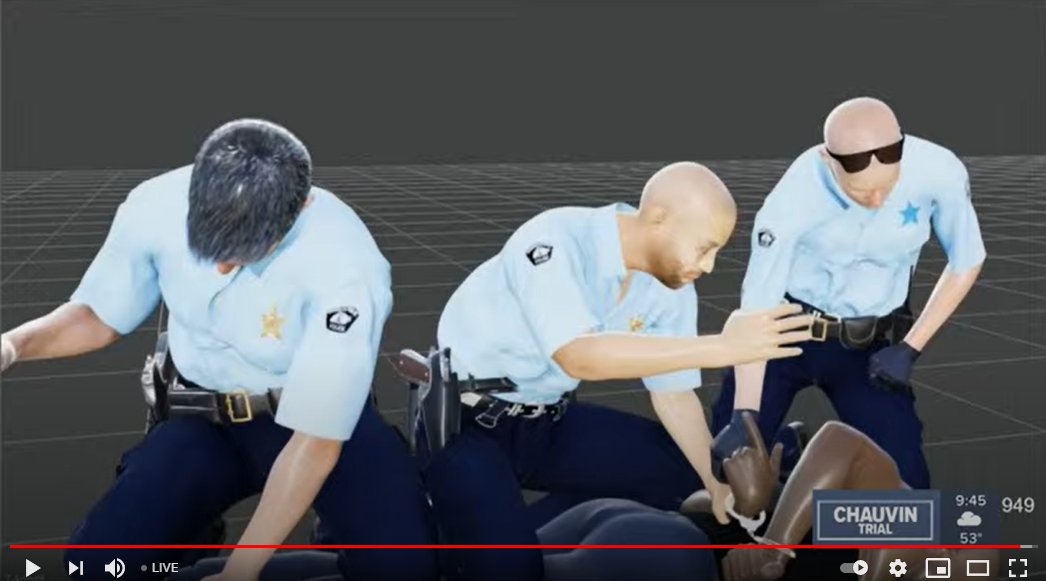
托宾分析了三名限制弗洛伊德的警察的图像,检察官说这差不多是9,1/2分钟,他证明了肖万的膝盖在90%的时间内“几乎在脖子上”。去年5月25日,肖万和其他三名警察逮捕弗洛伊德,理由是他涉嫌使用一张20美元假钞。肖万将戴着手铐的弗洛伊德压在地面上,膝盖跪在后者颈部,这一过程被一名旁观者录下并发布在网络上。弗洛伊德之死被视为警察如何对待美国黑人的象征,并引发全球范围内反对种族不公的抗议。
他说,其他几个因素也使弗洛伊德难以呼吸:警官抬起嫌疑犯的手铐,坚硬的人行道,俯卧位,转过头和膝盖。托宾说,在弗洛伊德最后一口气之后,乔万将膝盖保持在弗洛伊德脖子上3分钟2秒钟。 最后一口气之后,弗洛伊德的氧气水平降至零,弗洛伊德“达到了体内没有一盎司氧气的地步,”他说。
检察官在地上反复播放弗洛伊德的视频片段时,托宾指出了他所说的那张面孔的变化,告诉他弗洛伊德已死。 那一刻发生在警察开始压制弗洛伊德后大约五分钟。托宾说:“起初,您可以看到他的意识,可以看到轻微的闪烁,然后消失。” 他解释说:“那是生命从他的身体中消失的时刻。”
他在人体摄影机镜头中突出显示了弗洛伊德的双腿向空中抬起的那一刻。 托宾说,这种非自愿运动也称为缺氧性癫痫发作,是由于缺氧导致致命的脑损伤的证据。托宾撰写了有关机械通气的教科书,他直接向陪审团表示,并鼓励他们在描述呼吸的原理时感觉自己的脖子和胸部。 根据法庭内部的汇总报告,几乎所有陪审员都按照医生的要求做,并与证词紧密联系。
医学检查员安德鲁·贝克(Andrew Baker)博士曾为弗洛伊德进行尸检,他表示,他仍然坚持自己最初的判断,将弗洛伊德的死亡归类为他杀。对于肖万的辩护律师“弗洛伊德死于药物和生前健康状况”的说法,贝克表示,弗洛伊德的心脏病和芬太尼的使用是导致他死亡的因素,但它们不是直接原因,在死亡证明上这些因素只能被列为“其他重要条件”。
法医病理学家林赛·托马斯博士(Dr. Lindsey Thomas)表示,她同意贝克在死因上的判断,并补充说,她认为“主要造成死亡的机制是窒息或缺氧”。托马斯表示,弗洛伊德被束缚时的位置导致其“无法获得足够的氧气”来支持他的身体功能,她认为,执法人员“制服、束缚和颈部压迫的行为”导致了弗洛伊德的死亡。
NMS实验室的法医毒物学家丹尼尔·伊森施密德(Daniel Isenschmid)周四下午作证说,他死后在弗洛伊德(Floyd)的血液中发现了一些药物。
测试发现,弗洛伊德的血液中每毫升芬太尼含有约11纳克。 艾森施密德说,这与因酒后驾车而被捕的人的水平相当,但低于死后接受测试的人的水平。 他说,由于耐受性,芬太尼对某人的影响可能因人而异。据艾森施密德说,弗洛伊德体内每毫升甲基苯丙胺也有19纳克,这是一个“非常低”的水平。一天前,陪审员听到证词,在弗洛伊德的车中发现了几片含有芬太尼和甲基苯丙胺的白色药丸,在警车的后部发现了一块装有弗洛伊德唾液的小药丸。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#药物使用#
24
#非心脏#
39
🛖
59
学习了
62
好文章!
65